Abstract
Background
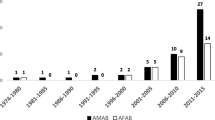
Over the last 6 years, there has been a change in the demographics of people presenting to gender services in Ireland. This is in line with international trends describing a higher number of transgender men (Female-Male, FTM, AFAB) presenting to gender services as compared to transgender women (Male–Female, MTF, AMAB), and lower ages at referral. Given the changes in demographics, it would be anticipated that clinical needs may have changed. This study describes the demographics of a young Irish sample (participants aged 18–30 years old) and explores the referral pathways and clinical needs of this cohort.
Methods
The study was performed as a retrospective chart review of 167 charts at The National Gender Service in Ireland over a five-month period.
Results
Transgender men represented 62.3% of the sample, transgender women 35.3%, and transmasculine/non-binary individuals represented 2.4%. Over two-thirds of participants were on gender affirming hormone therapy or GnRH antagonists and 16.1% had undergone surgical interventions. The median time from referral received to being seen at the clinic was 450 days (481 mean). Mental health comorbidities remain high with 49.1% of youth experiencing depression, a further 15.6% low mood and 26.3% anxiety.
Conclusion
This is the first study to show increasing referrals of people who were assigned female at birth (AFAB) over assigned male at birth (AMAB) individuals in Ireland, and to document the clinical needs of this cohort. By understanding the changing demographics and clinical needs, we can better plan for care and service improvements.


Similar content being viewed by others
References
Coleman E, Bockting W, Botzer M et al (2012) Standards of care for the health of transsexual, transgender, and gender- nonconforming people Version. 7. Int J Transgend 13(4):165–232. https://doi.org/10.1080/15532739.2011.700873
Institute of Medicine (US) Committee on lesbian, gay, bisexual, and transgender health issues and research gaps and opportunities (2011) The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington (DC): National Academies Press (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK64806. Accessed 15 Jan 2022. https://doi.org/10.17226/13128. pmid:22013611
Vijlbrief A, Saharso S, Ghorashi H (2020) Transcending the gender binary: gender non-binary young adults in Amsterdam. J LGBT Youth 17(1):89–106. https://doi.org/10.1080/19361653.2019.1660295
American Psychological Association (2015) Guidelines for psychological practice with transgender and gender nonconforming people. Am Psychol 70(9):832–864. https://doi.org/10.1037/a0039906
Vance SR, Ehrensaft D, Rosenthal SM (2014) Psychological and medical care of gender nonconforming youth. Pediatrics 134(6):1184–1192. https://doi.org/10.1542/peds.2014-0772
McNeil J, Bailey L, Ellis SJ, Regan M (2013) Speaking from the margins: trans mental health and wellbeing in Ireland. Transgender Equality Network Ireland (TENI)
T’Sjoen G, Arcelus J, Gooren L et al (2018) Endocrinology of transgender medicine. Endocr Rev 40(1):97–117. https://doi.org/10.1210/er.2018-00011
Sutcliffe PA, Dixon S, Akehurst RL et al (2009) Evaluation of surgical procedures for sex reassignment: a systematic review. J Plast Reconstr Aesthetic Surg. 62(3):294–306. https://doi.org/10.1016/j.bjps.2007.12.009
Zucker KJ (2017) Epidemiology of gender dysphoria and transgender identity. Sex Health 14(5):404–411. https://doi.org/10.1071/SH17067
Judge C, Donovan CO, Callaghan G et al (2014) Gender dysphoria – prevalence and co-morbidities in an Irish adult gender dysphoria – prevalence and co-morbidities in an Irish adult population. Front Endocrinol. https://doi.org/10.3389/fendo.2014.00087
Arcelus J, Bouman WP, Van Den Noortgate W et al (2015) Systematic Review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry 30(6):807–815. https://doi.org/10.1016/j.eurpsy.2015.04.005
Herman JL, Flores AR, Brown TNT et al (2017) Age of individuals who identify as transgender in the United States. Los Angeles, CA: The Williams Institute
Kaltiala-Heino R, Lindberg N (2019) Gender identities in adolescent population: Methodological issues and prevalence across age groups. Eur Psychiatry 55:61–66. https://doi.org/10.1016/j.eurpsy.2018.09.003
Kearns S, Kroll T, O‘Shea D, Neff K (2021) Experiences of transgender and non-binary youth accessing gender-affirming care: a systematic review and meta-ethnography. PLoS ONE 16(9):e0257194. https://doi.org/10.1371/journal.pone.0257194
Quilty A, Norris M (2020) A qualitative study of LGBTQI+ youth homelessness in Ireland. Available at: https://belongto.org/wp-content/uploads/2020/09/LGBTQI-Youth-Homelessness-Report_FINAL-VERSION.pdf. Accessed 15 Jan 2022
Olson J, Schrager SM, Belzer M et al (2015) Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. J Adolesc Heal 57(4):374–380. https://doi.org/10.1016/j.jadohealth.2015.04.027
Olson KR, Durwood L, Demeules M, McLaughlin KA (2016) Mental health of transgender children who are supported in their identities. Pediatrics. https://doi.org/10.1542/peds.2015-3223
Heard J, Morris A, Kirouac N et al (2018) Gender dysphoria assessment and action for youth: review of health care services and experiences of trans youth in Manitoba. Paediatr Child Heal 23(3):179–184. https://doi.org/10.1093/pch/pxx156
Anderssen N, Sivertsen B, Lønning KJ, Malterud K (2020) Life satisfaction and mental health among transgender students in Norway. BMC Public Health 20(1):1–11. https://doi.org/10.1186/s12889-020-8228-5
Becerra-Culqui TA, Liu Y, Nash R et al (2018) Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics. https://doi.org/10.1542/peds.2017-3845
Butler G, De Graaf N, Wren B, Carmichael P (2018) Assessment and support of children and adolescents with gender dysphoria. Arch Dis Child 103(7):631–636. https://doi.org/10.1136/archdischild-2018-314992
Arnoldussen M, Steensma TD, Popma A et al (2019) Re-evaluation of the Dutch approach: are recently referred transgender youth different compared to earlier referrals? Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-019-01394-6
Goldberg AE, Kuvalanka K, Dickey L (2019) Transgender graduate students’ experiences in higher education: A mixed-methods exploratory study. J Divers High Educ. 12(1):38–51. https://doi.org/10.1037/dhe0000074
Inwards-Breland DJ, Divall S, Salehi P et al (2019) Youth and parent experiences in a multidisciplinary gender clinic. Transgender Heal 4(1):100–106. https://doi.org/10.1089/trgh.2018.0046
Gridley SJ, Crouch JM, Evans Y et al (2016) Youth and caregiver perspectives on barriers to gender-affirming health care for transgender youth. J Adolesc Heal. https://doi.org/10.1016/j.jadohealth.2016.03.017
Pullen Sansfaçon A, Temple-Newhook J, Suerich-Gulick F et al (2019) The experiences of gender diverse and trans children and youth considering and initiating medical interventions in Canadian gender-affirming speciality clinics. Int J Transgenderism. 20(4):371–387. https://doi.org/10.1080/15532739.2019.1652129
Riggs DW, Bartholomaeus C, Sansfaçon AP (2019) ‘If they didn’t support me, I most likely wouldn’t be here’: transgender young people and their parents negotiating medical treatment in Australia. Int J Transgenderism. https://doi.org/10.1080/15532739.2019.1692751
Carlile A (2019) The experiences of transgender and non-binary children and young people and their parents in healthcare settings in England, UK: Interviews with members of a family support group. Int J Transgenderism. https://doi.org/10.1080/15532739.2019.1693472
Higgins A, Downes C, Murphy R et al (2016) The LGBT Ireland Report: The national study of the mental health and wellbeing of lesbian, gay, bisexual, transgender and intersex people in Ireland. Dublin, Ireland: Gay and Lesbian Equality Network (GLEN) and BeLonG To Youth Services
McCann E (2015) Transgender mental health. J Psychiatr Ment Health Nurs 22:76–81. https://doi.org/10.1111/jpm.12190
Warrier V, Greenberg DM, Weir E et al (2020) Elevated rates of autism, other neurodevelopmental and psychiatric diagnoses, and autistic traits in transgender and gender-diverse individuals. Nat Commun 11(1):1–12. https://doi.org/10.1038/s41467-020-17794-1
Department of Health (2018) Estimating prevalence of autism spectrum disorders (ASD) in the Irish population. Dublin: Irish Department of Health. Available at: https://assets.gov.ie/10707/ce1ca48714424c0ba4bb4c0ae2e510b2.pdf. Accessed 15 Jan 2022
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Sean Kearns. The first draft of the manuscript was written by Sean Kearns and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was collected by two clinical audits (2512 and 2513) and as such was approved by St Vincent’s University Hospital audit committee and conducted in accordance to the revised Helsinki Declaration.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kearns, S., O’Shea, D. & Neff, K. Transgender and non-binary demographics, referrals, and comorbidities among young Irish adults (2014–2020). Ir J Med Sci 192, 1679–1685 (2023). https://doi.org/10.1007/s11845-022-03163-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03163-y