Abstract
Background
With blood products being a limited and expensive resource within the healthcare system, there is an ever-increasing emphasis on judicial and appropriate use.
AIMS
To evaluate whether implementing contemporary society recommendations on restrictive transfusion policies would reduce inappropriate use of red blood cell transfusions, by evaluating the effect of a staff educational campaign.
Methods
An audit of peri-partum red cell concentrate (RCC) transfusion practice within a tertiary obstetric unit was undertaken, covering a 1-year period (2015), examining data related to transfusion prescribing practices. Subsequently, an educational programme was held for clinical and laboratory staff which aimed to bring practice in line with society guidelines. A repeat audit covering another 1-year period (2018) was undertaken.
Results
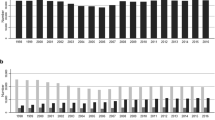
The number of RCC units of transfused reduced by 49% between 2015 and 2018 (426 to 218). The number of patients receiving transfusion dropped from 166 in 2018 (1.8% of births) to 119 in 2015 (1.5% of births). Among stable patients who were transfused, the proportion receiving a single unit increased from 6.9 to 53.9%. (p < 0.001). Haematological reassessment between units rose from 13.8 to 80.4% (p < 0.001). Written consent documentation improved (68% in 2018 vs. 38% in 2015) (p < 0.001).
Conclusions
The implementation of guidelines has resulted in substantial reduction in RCC transfusions between 2015 and 2018. Fewer women received a blood transfusion, and those who did received fewer units. There is a higher proportion of patients being reassessed between units and receiving single unit transfusions. Recording of consent has improved.

Similar content being viewed by others
References
Shander A, Isbister J, Gombotz H (2016) Patient blood management: the global view. Transfusion 56(suppl 1):S94-102
Delaney M, Wendel S, Bercovitz R et al (2016) Transfusion reactions: prevention, diagnosis, and treatment. Lancet 388(10061):2825–2836
Carson JL, Guyatt G, Heddle NM et al (2016) Clinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA 316:2025–35
The National Institute for Health and Care Excellence (2015) Blood transfusion NICE guideline [NG24], November 2015. Available at: https://www.nice.org.uk/guidance/ng24. Retrieved 22 Jan 2020
Green L, Connolly C, Choo G. (2015) Blood Transfusion in Obstetrics (Green-top Guideline No. 47).[ebook] Royal College of Obstetricians & Gynaecologists. Available at: https://www.rcog.org.uk/guidance/browse-all-guidance/green-top-guidelines/blood-transfusions-in-obstetrics-green-top-guideline-no-47/. Retrieved 22 Jan 2020
National Blood Authority (NBA) (2015) Patient blood management guidelines: Module 5 – Obstetrics and Maternity. Canberra, Australia
Holst LB, Petersen MW, Haase N et al (2015) Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. BMJ 350:h1354
Garrioch M, Sandbach J, Pirie E et al (2004) Reducing red cell transfusion by audit, education and a new guideline in a large teaching hospital. Transfus Med 14:25–32
Mayson E, Shand AW, Ford JB (2016) Single-unit transfusions in the obstetric setting: a qualitative study. Transfusion 56:1716–1722
So-Osman C, Cicilia J, Brand A et al (2010) Triggers and appropriateness of red blood cell transfusions in the postpartum patientâ⃞“a retrospective audit. Vox Sang 98(1):65–69
Stephens B, Sethna F, Crispin P (2017) Postpartum obstetric red cell transfusion practice: a retrospective study in a tertiary obstetric centre. Aust NZ J Obstet Gy 58(2):170–177
Butwick A, Aleshi P, Fontaine M et al (2009) Retrospective analysis of transfusion outcomes in pregnant patients at a tertiary obstetric center. Int J Obstet Anesth 18(4):302–308
Parker J, Thompson J, Stanworth S (2009) A retrospective one-year single-centre survey of obstetric red cell transfusions. Int J Obstet Anesth 18(4):309–313
Silverman JA, Barrett J, Callum JL (2004) The appropriateness of red blood cell transfusions in the peripartum patient. Obstet Gynecol 104:1000–1004
Catling S (2007) Blood Conservation techniques in obstetrics: a UK perspective. Int J Obstet Anesth 16:241–249
Shandar A (2012) Proceedings from the National Summit of Overuse. The Joint Commission and American Medical Association Convened Physician Consortium for Performance Improvement. Published 2012. Available at: http://www.jointcommission.org/assets/1/6/national_summit_overuse.pdf. Retrieved 17 Jan 2020
Vetter TR, Lalleh F. John R et al (2014) Perceptions about blood transfusion. Anesth Analg 118(6):(1301–1308)
Finucane ML, Slovic P, Mertz CK (2000) Public perception of the risk of blood transfusion. Transfusion 40:1017–1022
Ibrahim I, Sun D (2012) The cost of blood transfusion in Western Europe as estimated from six studies. Transfusion 52(9):1983–1988
Franchini M, Marano G, Mengoli C et al (2017) Red blood cell transfusion policy: a critical literature review. Blood Transfus 15:307–317
Simancas-Racines D, Montero-Oleas N, Vernooij RWM et al (2019) Quality of clinical practice guidelines about red blood cell transfusion. J Evid Based Med 12:113–124
Dahlke JD, Mendez-Figueroa H, Maggio L et al (2015) Prevention and management of postpartum hemorrhage: a comparison of 4 national guidelines. Am J Obstet Gynecol 213(76):e1-10
Munoz M, Stensballe J, Ducloy-Bouthors AS et al (2019) Patient blood management in obstetrics: prevention and treatment of postpartum haemorrhage. A NATA consensus statement. Blood Transfus 17(2):112–136
American College of Obstetricians and Gynecologists (2017) Practice Bulletin No. 183: Postpartum Hemorrhage. Obstet Gynecol 130(4):e168-e186
Leduc D, Senikas V, Lalonde AB et al (2009) Clinical practice obstetrics committee; society of obstetricians and gynaecologists of Canada. Active management of the third stage of labour: prevention and treatment of postpartum hemorrhage. J Obstet Gynaecol Can 31:980–993
Patterson JA, Roberts CL, Isbister JP et al (2015) What factors contribute to hospital variation in obstetric transfusion rates? Vox Sang 108(1):37–45
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
As an audit of routine clinical practice, this study was exempt from institutional research board/ethics review.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kelly, S., Sharpe, S., Culliton, M. et al. The effect of clinician education on blood transfusion practice in obstetrics: completing the audit cycle. Ir J Med Sci 192, 765–771 (2023). https://doi.org/10.1007/s11845-022-03032-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03032-8