Abstract
Background
Diabetic foot ulceration (DFU) has become an increasingly common emergency presentation. These patients are presenting at a younger age and with increasingly complex co-morbidities. They require frequent hospitalisation for management of DFU which has significant consequences for management of health resources but also for quality of life in the diabetic patient population.
Aim
The aim of this study was to evaluate the impact of the development of a coordinated, streamlined acute diabetic foot pathway for management of in-patients presenting as emergencies with DFU on length of stay, re-admission to hospital and minor and major amputations.
Methods
A dedicated acute diabetic foot pathway was introduced to St. Vincent’s University Hospital (SVUH) in April 2016. Management of patients admitted urgently to the emergency department or out-patient clinics of St. Vincent’s University Hospital during the 3-year period before April 2016 was compared to that of patients admitted in the 3 years after April 2016 following introduction of the acute diabetic foot pathway. Demographic data hospital length of stay, need for re-admission, major and minor amputations performed and cost of hospital stay were compared before and after introduction of the pathway.
Results
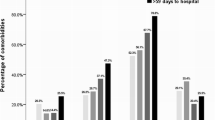
There were 931 admissions with acute diabetic foot ulceration or infection between January 2012 and December 2019; 419 were admitted between January 2012 and March 2016 and 512 between April 2016 and December 2019. There was no difference in demographic data between the two time periods. Length of stay decreased from 13 +/- 4.24 to 3 +/- 1.41 days between the two time periods (p < 0.001). Re-admission rates within 30 days decreased from 21.7 to 10.1% (p < 0.05). The number of major lower limb amputations decreased over the two time periods from 8.8 to 7.2% with a concomitant increase in minor amputations from 16.7 to 25.3%. Risk of major lower limb amputation was significantly higher in those patients living more than 20 km from the hospital. Costs associated with in-patient stay for management of DFU decreased from €9,247,700 to €8,988,100 despite an 18% increase in the number of patients treated and a 9.9% increase in hospital admissions.
Conclusion
Introduction of a dedicated, streamlined pathway involving multi-disciplinary input resulted in a significant improvement in patient management as assessed by length of hospital stay and need for re-admission. While the number of major lower limb amputations has decreased there has been a significant increase in the number of minor amputations.






Similar content being viewed by others

References
Forde H, Wrigley S, O’Murchadha LT et al (2020) Five-year outcomes of patients attending a diabetic foot clinic in a tertiary referral centre. Ir J Med Sci 189(2):511–515. https://doi.org/10.1007/s11845-019-02108-2. (Epub 2019 Oct 24)
Tracey ML, McHugh SM, Buckley CM et al (2016) The prevalence of Type 2 diabetes and related complications in a nationally representative sample of adults aged 50 and over in the Republic of Ireland. Diabet Med 33(4):441–445. https://doi.org/10.1111/dme.12845. (Epub 2015 Aug 16PMID: 26112979)
Health Service Executive (2011) Model of Care for the diabetic foot. National Diabetes Working Group. Dublin: HSE
Buckley CM, O’Farrell A, Canavan RJ et al (2012) Trends in the incidence of lower extremity amputations in people with and without diabetes over a five-year period in the Republic of Ireland. PLoS One 7(7):e41492
Canavan RJ, Unwin NC, Kelly WF, Connolly VM (2008) Diabetes- and non-diabetes-related lower extremity amputation incidence before and after the introduction of better organised diabetes foot care: continuous longitudinal monitoring using a standard method. Diabetes Care 31(3):459–63
Hingorani A, LaMuraglia GM, Henke P et al (2016) The management of diabetic foot: a clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg 63:3S-21S
Frykberg RG, Zgonis T, Armstrong DG et al (2006) A clinical practice guideline (2006 revision). J Foot Ankle Surg 45(Suppl):S1–66. Diabetic foot disorders
Kerr M, Barron E, Chadwick P et al (2019) The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med 36:995–1002
Sumpio BE, Armstrong DG, Lavery LA et al (2010) The role of interdisciplinary team approach in the management of the diabetic foot: a joint statement from the society for vascular surgery and the American Podiatric Medical Association. J Vasc Surg 51(6):1504–06
Prompers L, Huijberts M, Apelqvist J et al (2007) High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the EURODIALE study. Diabetoligia 50:18–25
Prompers L, Schaper N, Apelqvist I et al (2008) Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study Diabetologia 51:747–755
McKee M, Priest P, Ginzier M, Black N (1991) Which general surgical operations must be done at night? Ann R Coll Surg 73:295–302
Nason GJ, Strapp H, Kiernan C et al (2013) The cost utility of a multi-disciplinary foot protection clinic (MDFPC) in an Irish hospital setting. Ir J Med Sci 192(1);41–6
Krishnan S, Nash F, Baker N et al (2008) Reduction in diabetic amputations over 11 years in a defined UK population: benefits of multidisciplinary team work and continuous prospective audit. Diabetes Care 31(1):99–101
Musuuza J, Sutherland BL, Kurter S et al (2020) A systematic review of multi-disciplinary teams to reduce major amputations for patients with diabetic foot ulcers. J Vasc Surg 71(4):1433–1446
Doyle S, Bourke M, Kellegher E et al (2020) Ten year audit of outcomes following digital amputation. Ir J Med Sci 189(Suppl 5)S119
Hsu CR, Chang CC, Chen YT et al. (2016) Organisation of wound healing services: the impact on lowering the diabetes foot amputation rate in a ten-year review and the importance of early debridement. Diabetes Res Clin Pract 109(1):77–84
Gallagher D, Jordan V, Gillespie P et al (2014) Distance as a risk factor for amputation in patients with diabetes: a case-control study. Ir Med J 107(4)107–109
Delea S, Buckley C, Hanrahan A et al (2015) Management of diabetic foot disease and amputation in the Irish health system: a qualitative study of patients’ attitudes and experiences with health services. BMC Health Serv Res 1(15):251. https://doi.org/10.1186/s12913-015-0926-9
Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 14:1418–1428
Ambler GK, Kotta PA, Zielinski L et al (2020) The effect of frailty on long term outcomes in vascular surgical patients. EJVES 60:264–272
Jackson BM, Nathan DP, Doctor L et al (2011) Low rehospitalization rate for vascular surgery patients. J Vasc Surg 54(3):767–772
Beaulieu RJ, Grimm JC, Lyu H (2015) Abularrage CJ Perler BA, Prediction for readmission and reamputation following minor lower extremity amputation. J Vasc Surg 62(1):101–105
Brem H, Sheehan P, Rosenberg JH et al (2006) Evidence-based protocol for diabetic foot ulcers. Plast Reconstr Surg 117(7Suppl):193S-209S
Huang DY, Wilkins CJ, Evans DR et al (2004) The diabetic foot: the importance of coordinated care. Semin Intervent Radiol 31(4):307–312
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study received approval from the Clinical Audit Committee of St. Vincent’s University Hospital.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hurley, H., Kellegher, E., Gallen, T. et al. Development of a coordinated acute diabetic foot pathway for management of acute diabetic foot infection and ulceration. Ir J Med Sci 192, 161–167 (2023). https://doi.org/10.1007/s11845-022-02935-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-02935-w