Abstract
Background
Medication errors remain one of the most common types of incidents reported in Australian hospitals. Studies have reported that for every 10 medication administrations, a medication administration error is likely to occur and reach the patient, potentially contributing to a preventable patient harm.
Objective
To assess the impact of a mixed intervention model on medication administration errors in an Australian hospital.
Methods
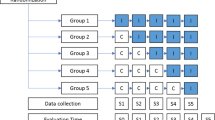
Two types of intervention model (human and system orientated) were implemented through collaboration with key stakeholders (nurses, educators, and policy makers) to reduce medication administration errors across this 650-bed multisite Australian hospital from August 2018 to June 2019. To assess the impact of the mixed intervention model, the total number of reported medication errors and the number of medication administration errors were retrieved from the hospital electronic medication management system for 12 months before (from June 2017 to July 2018) and after (from July 2019 to June 2020) implementation of all interventions.
Results
Implementation of a mixed intervention model through collaboration with stakeholders resulted in significant reduction in the number of medication administration errors, and those with harm (from 68 to 55%, P < 0.0001 and from 12 to 8%, P = 0.0001 respectively). Additionally, the severity of medication administration errors was also reduced (HR 0.562, 95% CI (0.298–1.062)) in the post-intervention phase.
Conclusion
Introducing a mixed intervention model reduces medication administration errors across health settings and has the potential to drive excellence in healthcare.

adapted from Journal of Pharmacy Practice and Research)9
Similar content being viewed by others
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Australian Commission on Safety and Quality in Health Care (2020) The National Safety and Quality Hospital (NSQHS) Standards June 2020. [cited 2020 Jun 26th] Available from: https://www.safetyandquality.gov.au/standards/nsqhs-standards
Roughead EE, Semple SJ, Rosenfeld E (2016) The extent of medication errors and adverse drug reactions throughout the patient journey in acute care in Australia. Int J Evid Based Healthc 14(3):113–122. https://doi.org/10.1097/XEB.0000000000000075
Australian Commission on Safety and Quality in Healthcare (ACQS) (2013) Evidence briefings on interventions to improve medication. Vol 1(3). [Cited 2020 Jun 29th] Available on: https://www.safetyandquality.gov.au/sites/default/files/migrated/Evidence-briefings-on-interventions-to-improve-medication-safety-Double-checking-medication-administration-PDF-888KB.pdf
Küng K, Aeschbacher K, Rütsche A et al (2017) Frequency of medication preparation and medication administration errors in a Swiss university hospital. A prospective observational study] Pflege 30(6):329–338. https://doi.org/10.1024/1012-5302/a000546
Riaz MK, Riaz M, Latif A (2017) Review - Medication errors and interventions for their prevention. Pak J Pharm Sci 30(3):921–928
Keers RN, Plácido M, Bennett K et al (2018) What causes medication administration errors in a mental health hospital? A qualitative study with nursing staff. PLoS ONE 13(10):e0206233. https://doi.org/10.1371/journal.pone.0206233
Zhou S, Kang H, Yao B et al (2018) Analyzing medication error reports in clinical settings: an automated pipeline approach. AMIA Annu Symp Proc 2018:1611–1620. Published 2018 Dec 5
Ferner RE, Aronson JK (2006) Clarification of terminology in medication errors: definitions and classification. Drug Saf 29(11):1011–1022. https://doi.org/10.2165/00002018-200629110-00001 (PMID: 17061907)
Stowasser DA, Alllinson YM, O’leary KM (2004) Understanding the medicines management pathway. J Pharm Pract Res 34(4)
Chen Y, Wu X, Huang Z et al (2019) Evaluation of a medication error monitoring system to reduce the incidence of medication errors in a clinical setting. Research in social & administrative pharmacy: RSAP 15(7):883–888. https://doi.org/10.1016/j.sapharm.2019.02.006
Huckels-Baumgart S, Niederberger M, Manser T et al (2017) A combined intervention to reduce interruptions during medication preparation and double-checking: a pilot-study evaluating the impact of staff training and safety vests. J Nurs Manag 25(7):539–548. https://doi.org/10.1111/jonm.12491
Institute for Safe Medication Practices (ISMP) (2020) ISMP targeted medication safety best practices for hospitals. (cited on the 29th June) Available at: https://www.ismp.org/guidelines/best-practices-hospitals
Khalil H, Lee S (2018) The implementation of a successful medication safety program in a primary care. J Eval Clin Pract 24(2):403–407. https://doi.org/10.1111/jep.12870
Al Tehewy M, Fahim H, Gad NI et al (2016) A Medication administration errors in a university hospital. J Patient Saf 12(1):34–39. https://doi.org/10.1097/PTS.0000000000000196
Bifftu BB, Mekonnen BY (2020) The magnitude of medication administration errors among nurses in Ethiopia: a systematic review and meta-analysis. Int J Caring Sci 9(1):1–8. https://doi.org/10.34172/jcs.2020.001
Berdot S, Gillaizeau F, Caruba T et al (2013) Drug administration errors in hospital inpatients: a systematic review. PLoS ONE 8(6):e68856. https://doi.org/10.1371/journal.pone.0068856
Berdot S, Sabatier B, Gillaizeau F et al (2012) Evaluation of drug administration errors in a teaching hospital. BMC hospitals research 12:60. https://doi.org/10.1186/1472-6963-12-60
Koyama AK, Maddox CS, Li L et al (2020) Effectiveness of double checking to reduce medication administration errors: a systematic review. BMJ Qual Saf 29(7):595–603. https://doi.org/10.1136/bmjqs-2019-009552
Lapkin S, Levett-Jones T, Chenoweth L et al (2016) The effectiveness of interventions designed to reduce medication administration errors: a synthesis of findings from systematic reviews. J Nurs Manag 24(7):845–858. https://doi.org/10.1111/jonm.12390
Leahy IC, Lavoie M, Zurakowski D et al (2018) Medication errors in a pediatric anesthesia setting: incidence, etiologies, and error reduction interventions. J Clin Anesth 49:107–111. https://doi.org/10.1016/j.jclinane.2018.05.011
Institute of Medicine (2006) http://www.iom.edu/Reports/2006/Preventing-Medication-Errors-Series.aspx. Released July 20, 2006. Accessed 8th February 2021
Ofusu R, Jarrett P (2015) Reducing nurse medicine administration errors. Nursing Times 111(20):12–14. https://www.nursingtimes.net/clinical-archive/medicine-management/reducing-nurse-medicine-administration-errors-11-05-2015/
Contents RJ (1990) In: Human error. Cambridge University Press, Cambridge, pp ix–x
Reason J (1997) Managing the risks of organizational accidents. London: Routledge. https://doi.org/10.4324/9781315543543
Wondmieneh A, Alemu W, Tadele N, Demis A (2020) Medication administration errors and contributing factors among nurses: a cross sectional study in tertiary hospitals, Addis Ababa, Ethiopia. BMC nursing 19(1):1–9. https://doi.org/10.1186/s12912-020-0397-0
Khalil H (2015) Implementing change in healthcare: evidence utilization. Int J Evid Based Healthc 13(2):41–42. https://doi.org/10.1097/XEB.0000000000000045
Keers RN, Williams SD, Cooke J et al (2013) Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf 36(11):1045–1067. https://doi.org/10.1007/s40264-013-0090-2
Khalil H, Shahid M, Roughead L (2017) Medication safety programs in primary care: a scoping review. JBI Database Syst Rev Implement 15(10):2512–2526. https://doi.org/10.11124/JBISRIR-2017-003436
Khalil H (2019) Successful implementation of a medication safety program for aboriginal health practitioners in rural Australia. Aust J Rural Health 27(2):158–163. https://doi.org/10.1111/ajr.12494
Durham ML, Suhayda R (2016) Reducing medication administration errors in acute and critical care. JONA 46(2):75–81
Bergström A, Ehrenberg A, Eldh AC et al (2020) The use of the PARIHS framework in implementation research and practice-a citation analysis of the literature. Implement Sci 15(1):68. Published 2020 Aug 27. https://doi.org/10.1186/s13012-020-01003-0
Hauer KE, Holmboe ES, Kogan JR (2011) Twelve tips for implementing tools for direct observation of medical trainees’ clinical skills during patient encounters. Med Teach 33(1):27–33. https://doi.org/10.3109/0142159X.2010.507710
Rietmeijer C, Huisman D, Blankenstein AH et al (2018) Patterns of direct observation and their impact during residency: general practice supervisors’ views. Med Educ 52(9):981–991. Advance online publication. https://doi.org/10.1111/medu.13631
Acknowledgements
The authors would like to acknowledge the great work and support of all nursing staff, nurse unit managers, Peninsula Health Safer care unit staff, operational and clinical directors who were part of the various projects that were developed and implemented as part of a hospital-wide medication safety program overseen by the lead author (VK).
Author information
Authors and Affiliations
Contributions
Study conception and design: VK. Data collection: VK & AB. Data analysis and interpretation: VK. Drafting of the article: VK. Critical revision of the article: VK & AB.
Corresponding author
Ethics declarations
Ethical consideration
This study received exemption from the hospital Human Research & Ethics Committee as it did not involve any participants, and hence informed consent was not required/needed. All authors approved publication of this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khalil, V., Bates, A. Assessing the impact of a mixed intervention model on the reduction of medication administration errors in an Australian hospital. Ir J Med Sci 191, 2433–2438 (2022). https://doi.org/10.1007/s11845-021-02872-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02872-0