Abstract
Background
Surgical site infection (SSI) is a possible postoperative complication. Preoperative application of antiseptics on the surgical site can decrease the rate of SSIs.
Aim
This study aimed to compare the efficacy of 0.2% chlorhexidine (CHX) and 10% Betadine (povidone-iodine) for perioral skin disinfection prior to oral surgical procedures.
Methods
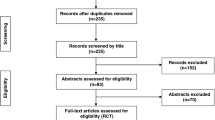
This clinical trial (IRCT20181017041365N1) (registration date: 2019/05/04) evaluated 57 male patients who were randomly selected among those presenting to the Periodontology Department of Ahvaz Jundishapur University. Baseline microbial samples were collected from the perioral skin at the right and left sides of the face in each patient by sterile swabs. Next, the perioral area was disinfected with 10% Betadine in the right side and 0.2% CHX in the left side. Secondary microbial samples were then collected. Wilcoxon matched-pairs signed-ranks and Mann–Whitney test were used to compare the colony counts. The significance level was set at p ≤ 0.05. Data were analyzed with the Stata program, version15.1.
Results
The bacterial colony count was 3147 (314,700) in the Betadine and 3139 (313,900) in the CHX group at baseline (P = 0.86). These values changed to 1196 (119,600) in the Betadine (P < 0.001) and 857 (85,700) in the CHX (P < 0.001) group after disinfection. A significant difference was found in colony count between the CHX and Betadine groups after intervention (P = 0.0001).
Conclusion
According to the results, 0.2% CHX has higher antimicrobial efficacy than 10% Betadine for perioral disinfection prior to oral surgical procedures.
Trial registration
IRCT20181017041365N1. Registered on 2019/05/04.

Similar content being viewed by others
Availability of data and materials
The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
De Lissovoy G, Fraeman K, Hutchins V et al (2009) Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 37(5):387–397
Ayoub F, Quirke M, Conroy R, Hill A (2015) Chlorhexidine-alcohol versus povidone-iodine for pre-operative skin preparation: a systematic review and meta-analysis. Int J Surg Open 1:41–46
Darouiche RO, Wall MJ Jr, Itani KM et al (2010) Chlorhexidine–alcohol versus povidone–iodine for surgical-site antisepsis. N Engl J Med 362(1):18–26
Lee I, Agarwal RK, Lee BY et al (2010) Systematic review and cost analysis comparing use of chlorhexidine with use of iodine for preoperative skin antisepsis to prevent surgical site infection. Infect Control Hosp Epidemiol 31(12):1219–1229
Hemani ML, Lepor H (2009) Skin preparation for the prevention of surgical site infection: which agent is best? Nat Rev Urol 11(4):190
Zhang D, Wang X-C, Yang Z-X et al (2017) RETRACTED: Preoperative chlorhexidine versus povidone-iodine antisepsis for preventing surgical site infection: A meta-analysis and trial sequential analysis of randomized controlled trials. Int J Surg 44:176–184
Cabral CT, Fernandes MH (2007) In vitro comparison of chlorhexidine and povidone–iodine on the long-term proliferation and functional activity of human alveolar bone cells. Clin Oral Investig 11(2):155–164
Gilbert P, Moore L (2005) Cationic antiseptics: diversity of action under a common epithet. J Appl Microbiol 99(4):703–715
Sidhwa F, Itani KM (2015) Skin preparation before surgery: options and evidence. Surg Infect 16(1):14–23
Rotter M (2001) Arguments for alcoholic hand disinfection. J Hosp Infect 48:S4–S8
Schwartz DM, Hurst GC, Kirk AM et al (2012) Reactive skin decontamination lotion (RSDL) for the decontamination of chemical warfare agent (CWA) dermal exposure. Curr Pharm Biotechnol 13(10):1971–1979
World Health Organization (2018) Global guidelines for the prevention of surgical site infection, 2nd ed. World Health Organization. https://apps.who.int/iris/handle/10665/277399
Chaiyakunapruk N, Veenstra DL, Lipsky BA, Saint S (2002) Chlorhexidine compared with povidone-iodine solution for vascular catheter–site care: a meta-analysis. Ann Intern Med 136(11):792-801
Barenfanger J, Drake C, Lawhorn J, Verhulst SJ (2004) Comparison of chlorhexidine and tincture of iodine for skin antisepsis in preparation for blood sample collection. J Clin Microbiol 42(5):2216–2217
Hsieh HF, Chiu HH, Lee FP (2006) Surgical hand scrubs in relation to microbial counts: systematic literature review. J Adv Nurs 55(1):68–78
Kenrad B (1990) Toxin effects from chlorhexidine gluconate: case report. Tandlaegebladet 94(12):489–491
Gezer S, Yalvaç HM, Güngör K, Yücesoy İ (2020) Povidone-iodine vs chlorhexidine alcohol for skin preparation in malignant and premalignant gynaecologic diseases: a randomized controlled study. Eur J Obstet Gynecol Reprod Biol 244:45–50
Raja SG, Rochon M, Mullins C et al (2018) Impact of choice of skin preparation solution in cardiac surgery on rate of surgical site infection: a propensity score matched analysis. Am J Infect Control 19(1):16–21
Ghobrial GM, Wang MY, Green BA et al (2018) Preoperative skin antisepsis with chlorhexidine gluconate versus povidone-iodine: a prospective analysis of 6959 consecutive spinal surgery patients. J Neurosurg Spine 28(2):209–214
Elshamy E, Ali YZ, Khalafallah M, Soliman A (2020) Chlorhexidine–alcohol versus povidone–iodine for skin preparation before elective cesarean section: a prospective observational study. J Matern Fetal Neonatal Med 33(2):272–276
Ritter B, Herlyn PKE, Mittlmeier T, Herlyn A (2020) Preoperative skin antisepsis using chlorhexidine may reduce surgical wound infections in lower limb trauma surgery when compared to povidone-iodine-a prospective randomized trial. Am J Infect Control 48(2):167–172
Lakhi NA, Tricorico G, Osipova Y, Moretti ML (2019) Vaginal cleansing with chlorhexidine gluconate or povidone-iodine prior to cesarean delivery: a randomized comparator-controlled trial. Am J Obstet Gynecol 1(1):2–9
Roeckner JT, Sanchez-Ramos L, Mitta M et al (2019) Povidone-iodine 1% is the most effective vaginal antiseptic for preventing post-cesarean endometritis: a systematic review and network meta-analysis. Am J Obstet Gynecol 221(3):261 e1-e20
Park H, Han S, Lee E et al (2017) Randomized clinical trial of preoperative skin antisepsis with chlorhexidine gluconate or povidone–iodine. Br J Surg 104(2):e145–e150
Davies B, Patel H (2016) Does chlorhexidine and povidone-iodine preoperative antisepsis reduce surgical site infection in cranial neurosurgery? Ann R Coll Surg Engl 98(6):405–408
Chen S, Chen JW, Guo B, Xu CC (2020) Preoperative antisepsis with chlorhexidine versus povidone-iodine for the prevention of surgical site infection: A systematic review and meta-analysis. World J Surg 44(5):1412–1424
Hadiati DR, Hakimi M, Nurdiati DS et al (2018) Skin preparation for preventing infection following caesarean section. Cochrane Database Syst Rev (10)
Privitera GP, Costa AL, Brusaferro S et al (2017) Skin antisepsis with chlorhexidine versus iodine for the prevention of surgical site infection: a systematic review and meta-analysis. Am J Infect Control 45(2):180–189
Acknowledgements
Not applicable.
Funding
This study was funded by Ahvaz University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by ND, NO, SSM, AFS, and KM. The first draft of the manuscript was written by SSM, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics declarations
Ethics approval
The study was approved by the ethics committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1397.264) and registered in the Iranian Registry of Clinical Trials (IRCT20181017041365N1). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dorestan, N., Ostadian, N., Mahmoudinezhad, S. et al. Comparative efficacy of 0.2% chlorhexidine and 10% Betadine for perioral skin disinfection prior to oral surgical procedures: a clinical trial. Ir J Med Sci 191, 2207–2211 (2022). https://doi.org/10.1007/s11845-021-02850-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02850-6