Abstract
Background
Emergence delirium occurs in children during recovery from general anesthesia. The aim of the study was to examine the effects of mask and intravenous sevoflurane anesthesia induction on emergence delirium in children undergoing tonsillectomy with or without adenoidectomy.
Methods
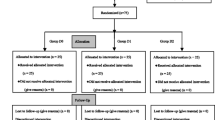
This single-blinded, prospective, randomized clinical trial was conducted in the operating room and the post-operative recovery area at a university hospital. Sixty-seven children (aged 3–12 years) were randomly assigned to receive either mask induction (group M) or intravenous induction (group IV). Vascular access was provided in group M after 8% sevoflurane and 60% nitrous oxide in oxygen were given through a mask. In the IV cohort, an intravenous cannula was inserted prior to induction. The incidence of emergence delirium was assessed using the Pediatric Anesthesia Emergence Delirium (PAED) scale after arrival in the post-anesthesia care unit. Post-operative pain was assessed using the Face, Legs, Activity, Cry, and Consolability (FLACC) scale.
Results
PAED scores were significantly higher in group M at 5 min (group M = 12.2 ± 4.215, group IV = 9.1 ± 4.0; mean difference = 3.094, 95% CI [1.108; 5.081]; P = 0.003), at 15 min (group M = 8.0 ± 2.6, group IV = 5.1 ± 2.3; mean difference = 2.942, 95% CI [1.586–4.301]; P < 0.001), and at 30 min (group M = 5.1 ± 2.8, group IV = 2.5 ± 1.8; mean difference = 2.620, 95% CI [1.457; 3.783]; P < 0.001) than in group IV. The FLACC scale scores were similar between the two groups.
Conclusion
Mask induction for pediatric patients undergoing tonsillectomy with or without adenoidectomy increased Pediatric Anesthesia Emergence Delirium scores more than intravenous induction.
Trial registration
NCT03252405


Similar content being viewed by others
References
Akihiro K (2016) Emergence agitation in children: risk factors, prevention, and treatment. J Anesth 30(2):261–267
Gooden R, Tennant I, James B et al (2014) The incidence of emergence delirium and risk factors following sevoflurane use in pediatric patients for day case surgery, Kingston, Jamaica. Rev Bras Anestesiol 64(6):413–418. https://doi.org/10.1016/j.bjan.2013.09.011
Card E, Pandharipande P, Tomes C et al (2015) Emergence from general anaesthesia and evolution of delirium signs in the post-anaesthesia care unit. Br J Anaesth 115:411
Bedirli N, Akçabay M, Emik U (2017) Tramadol vs dexmedetomidine for emergence agitation control in pediatric patients undergoing adenotonsillectomy with sevoflurane anesthesia: prospective randomized controlled clinical study. BMC Anesthesiol 17(1):41. https://doi.org/10.1186/s12871-017-0332-4
Costi D, Ellwood J, Wallace A, Ahmed S, Waring L, Cyna A (2015) Transition to propofol after sevoflurane anesthesia to prevent emergence agitation: a randomized controlled trial. Paediatr Anaesth 25:517–523
Driscoll JN, Bender BM, Archilla CA et al (2017) Comparing incidence of emergence delirium between sevoflurane and desflurane in children following routine otolaryngology procedures. Minerva Anestesiol 83(4):383–391. https://doi.org/10.23736/S0375-9393.16.11362-8
Chandler JR, Myers D, Mehta D, Whyte E, Groberman MK, Montgomery CJ, Ansermino JM (2013) Emergence delirium in children: a randomized trial to compare total intravenous anesthesia with intravenous anesthesia with propofol and remifentanil to inhalational sevoflurane anesthesia. Paediatr Anaesth 23(4):309–315. https://doi.org/10.1111/pan.12090
Choi EK, Lee S, Kim WJ et al (2018) Effects of remifentanil maintenance during recovery on emergence delirium in children with sevoflurane anesthesia. Paediatr Anaesth 28(8):739–744. https://doi.org/10.1111/pan.13446
Kain ZN, Caldwell-Andrews AA, Maranets I et al (2004) Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg 99:1648–1654
Beringer RM, Greenwood R, Kilpatrick N (2014) Development and validation of the Pediatric Anesthesia Behavior Score–an objective measure of behavior during induction of anesthesia. Paediatr Anaesth 24:196–200
Przybylo HJ, Tarbell SE, Stewenson GW (2005) Mask fear in children presenting for anesthesia: aversion, phobia or both? Paediatr Anaesth 15:366–370
Weldon BC, Watcha MF, White PF (1992) Oral midazolam in children: effect of time and adjunctive therapy. Anesth Analg 75:51–55
Sikich N, Lerman J (2004) Development and psychometric evaluation of the Pediatric Anesthesia Emergence Delirium scale. Anesthesiology 100:1138–1145
Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S (1997) The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs 23:293–297
Frederick HJ, Wofford K, Schulman SR (2016) A randomized controlled trial to determine the effect of depth of anesthesia on emergence agitation in children. Anesth Analg 122:1141–1146
Banchs JR, Lerman J (2014) Preoperative anxiety management, emergence delirium, and postoperative behavior. Anesthesiol Clin 32:1–23
Brioni JD, Varughese S, Ahmed R, Bein B (2017) A clinical review of inhalation anesthesia with sevoflurane: from early research to emerging topics. J Anesth 31(5):764–778. https://doi.org/10.1007/s00540-017-2375-6
Son JS, Jang E, Oh MW, Lee JH, Han YJ, Ko S (2015) A comparison of postoperative emergence agitation between sevoflurane and thiopental anesthesia induction in pediatric patients. Korean J Anesthesiol 68(4):373–378. https://doi.org/10.4097/kjae.2015.68.4.373
Lee CJ, Lee SE, Oh MK, Shin CM, Kim YJ, Choe YK, Cheong SH, Lee KM, Lee JH, Lim SH, Kim YH, Cho KR (2010) The effect of propofol on emergence agitation in children receiving sevoflurane for adenotonsillectomy. Korean J Anesthesiol 59(2):75–81. https://doi.org/10.4097/kjae.2010.59.2.75
Abu-Shahwan I (2008) Effect of propofol on emergence behavior in children after sevoflurane general anesthesia. Paediatr Anaesth 18(1):55–59
Jacobson AF, Winslow EH (2005) Variables influencing intravenous catheter insertion difficulty and failure: an analysis of 339 intravenous catheter insertions. Heart Lung 34:345–359
Lerwick JL (2016) Minimizing pediatric healthcare-induced anxiety and trauma. World J Clin Pediatr 5:143–150
Sommerfield D, von Ungern-Sternberg BS (2019) The mask or the needle? Which induction should we go for? Curr Opin Anesthesiol 32:377–383
Berghmans JM, Poley M, Weber F (2015) Does the Child Behavior Checklist predict levels of preoperative anxiety at anesthetic induction and postoperative emergence delirium? A prospective cohort study. Minerva Anestesiol 81(2):145–156
Hamer-Hodges RJ (1960) Induction of anaesthesia in young children. Lancet 1:82–87
Bal N, Saricaoglu F, Uzun S, Dal D, Celebi N, Celiker V, Aypar U (2006) Perioperative anxiety and postoperative behavioural disturbances in children: comparison between induction techniques. Eur J Anaesthesiol 23(6):470–475. https://doi.org/10.1017/S0265021506000408
Blankespoor RJ, Janssen NJ, Wolters AM et al (2012) Post-hoc revision of the pediatric anesthesia emergence delirium rating scale: clinical improvement of a bedside-tool? Minerva Anestesiol 78(8):896–900
Kotiniemi LH, Rhyanen PT (1996) Behavioural changes in children’s memories after intravenous, inhalation and rectal induction of anaesthesia. Paediatr Anaesth 6:201–217
Von Ungern-Sternberg BS, Boda K, Chambers NA et al (2010) Risk assessment for respiratory complications in paediatric anaesthesia: a prospective cohort study. Lancet 376:773–783
Ramgolam A, Hall GL, Zhang G et al (2018) Inhalational versus intravenous induction of anesthesia in children with a high risk of perioperative respiratory adverse events: a randomized controlled trial. Anesthesiology 128:1065–1074
Ortiz AC, Atallah AN, Matos D et al (2014) Intravenous versus inhalational anaesthesia for paediatric outpatient surgery. Cochrane Database Syst Rev 2:CD009015
Moore JK, Moore EW, Elliott RA, St Leger AS, Payne K, Kerr J (2003) Propofol and halothane versus sevoflurane in paediatric day-case surgery: induction and recovery characteristics. Br J Anaesth 90:461–466
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval for this study (2017-11/105) was provided by the Ethics Committee of the university’s Faculty of Medicine on June 20, 2017. Written consent was obtained from all the parents of the patients.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peker, K., Polat, R. Effects of intravenous and mask induction on post-operative emergence delirium in pediatric patients undergoing tonsillectomy with or without adenoidectomy. Ir J Med Sci 189, 1061–1068 (2020). https://doi.org/10.1007/s11845-020-02197-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02197-4