Abstract
Background
Double-J stents are used to treat ureteric outflow obstruction. Deployed in antegrade or retrograde fashion, they relieve ureteric obstruction in several conditions including ureteric calculi, strictures and malignancy. Traditionally exchanged in an operating theatre (OT) under general anaesthetic (GA), more recently described is the technique of using fluoroscopic guidance under sedation.
Aims
To assess the efficacy and safety of retrograde double-J stent exchange in an interventional radiology (IR) setting in a tertiary oncology referral centre over a 7-year period.
Methods
Clinical data on 460 double-J stent exchanges in 126 female patients was acquired from the hospital electronic patient record. Four fellowship-trained interventional radiologists performed the procedures. A standard approach was used in conjunction with conscious sedation using midazolam and fentanyl. Use of the technique with certain anatomical variations is also described.
Results
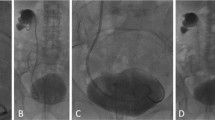
Technical success rate was 96%. The main reasons for failure included failure to snare the stent (1.8%) and patient discomfort (1.1%). The overall complication rate was 5%: 5 category 1 (minor) and 18 category 3 outcomes, with the latter group requiring further intervention. Average screening time was 9.65 min and the average radiation dose was 2018.24 mGy/m2. We also demonstrate the successful use of this method in patients with unusual anatomy and ileal conduits.
Conclusion
Fluoroscopic-guided retrograde double-J stent exchange is a safe and effective procedure that can be performed with a high degree of success using equipment and techniques used in daily IR practice. This approach precludes the need for GA, reduces OT utilisation and is well tolerated in a patient group for whom this procedure is typically palliative.






Similar content being viewed by others
Abbreviations
- EPR:
-
Electronic patient record
- GA:
-
General anaesthetic
- IR:
-
Interventional radiology
- PUJ:
-
Pelvi-ureteric junction
References
P. D. Zimskind, T. R. Fetter, and J. L. Wilkerson, “Clinical use of long-term indwelling silicone rubber ureteral splints inserted cystoscopically,” (in eng), J Urol, vol. 97, no. 5, pp. 840–844, 1967
H. A. Mitty, J. S. Train, and S. J. Dan, “Placement of ureteral stents by antegrade and retrograde techniques,” (in eng), Radiol Clin North Am, vol. 24, no. 4, pp. 587–600, 1986
R.-S. Chang et al., “Fluoroscopic guidance of retrograde exchange of ureteral stents in women,” American Journal of Roentgenology, vol. 190, no. 6, pp. 1665–1670, 2008/06/01 2008, doi: https://doi.org/10.2214/AJR.07.3216
J. W. Yedlicka, Jr., D. W. Aizpuru R Fau - Hunter, W. R. Hunter Dw Fau - Castaneda-Zuniga, K. Castaneda-Zuniga Wr Fau - Amplatz, and K. Amplatz, “Retrograde replacement of internal double-J ureteral stents,” (in eng), no. 0361-803X (Print), 19910517 DCOM- 19910517 1991
T. de Baere, A. Denys, P. Pappas, E. Challier, and A. Roche, “Ureteral stents: exchange under fluoroscopic control as an effective alternative to cystoscopy,” (in eng), Radiology, vol. 190, no. 3, pp. 887–889, 1994, doi: https://doi.org/10.1148/radiology.190.3.8115645
E. McCarthy et al., “Fluoroscopically guided transurethral removal and/or replacement of ureteric stents in women,” (in eng), Acta Radiol, vol. 56, no. 5, pp. 635–640, 2015, doi: https://doi.org/10.1177/0284185114533246
S. Sivalingam, I. Tamm-Daniels, and S. Y. Nakada, “Ambulatory and office urology: office-based ureteral stent placement under local anesthesia for obstructing stones is safe and efficacious,” Urology, Article vol. 81, pp. 498–502, 3/1/March 2013 2013, doi: https://doi.org/10.1016/j.urology.2012.10.021
S. W. Park et al., “Fluoroscopy-guided transurethral removal and exchange of ureteral stents in female patients: technical notes,” (in eng), J Vasc Interv Radiol, vol. 18, no. 2, pp. 251–256, 2007, doi: https://doi.org/10.1016/j.jvir.2006.12.722
R. F. Grasso, E. Faiella, R.L. Cazzato, G. Luppi, R. del Vescovo, F. Giurazza, S. Mercurio, B.B. Zobel, “Retrograde fluoroscopy-guided trans-urethral exchange of ureteral stents: comparison of direct grasping vs. modified snare,” (in eng), Indian J Radiol Imaging, vol. 23, no. 4, pp. 347–350, 2013, doi: https://doi.org/10.4103/0971-3026.125615
T. Kawahara et al., “Ureteral stent exchange under fluoroscopic guidance using the crochet hook technique in women,” (in eng), Urol Int, vol. 88, no. 3, pp. 322–325, 2012, doi: https://doi.org/10.1159/000336870
D. J. Mykulak, M. Herskowitz, and K. I. Glassberg, “Use of magnetic internal ureteral stents in pediatric urology: retrieval without routine requirement for cystoscopy and general anesthesia,” (in eng), J Urol, vol. 152, no. 3, pp. 976–977, 1994
O. Khalilzadeh et al., “Proposal of a new adverse event classification by the Society of Interventional Radiology Standards of Practice Committee,” (in eng), J Vasc Interv Radiol, vol. 28, no. 10, pp. 1432–1437.e3, 2017, doi: https://doi.org/10.1016/j.jvir.2017.06.019
O. Ozkan, D. Akinci, U. Bozlar, B. Ustunsoz, M. Ozmen, and O. Akhan, “Retrograde ureteral stent exchange under fluoroscopic guidance,” (in eng), Diagn Interv Radiol, vol. 15, no. 1, pp. 51–56, 2009
B. Gershman, B. H. Eisner, S. Sheth, and D. E. Sacco, “Ureteral stenting and retrograde pyelography in the office: clinical outcomes, cost effectiveness, and time savings,” (in eng), J Endourol, vol. 27, no. 5, pp. 662–666, 2013, doi: https://doi.org/10.1089/end.2012.0644
G. Carrafiello, D. Laganà, M. Mangini, C. Recaldini, M. Dizonno, A. Giorgianni, D. Lumia, A. Taborelli, S. Cuffari, C. Fugazzola, “Fluoroscopically guided retrograde replacement of ureteral stents,” (in eng ita), Radiol Med, vol. 112, no. 6, pp. 821–825, 2007, doi: https://doi.org/10.1007/s11547-007-0186-9
S. B. Gay, J. P. Armistead, M. E. Weber, and B. R. Williamson, “Left infrarenal region: anatomic variants, pathologic conditions, and diagnostic pitfalls,” (in eng), Radiographics, vol. 11, no. 4, pp. 549–570, 1991, doi: https://doi.org/10.1148/radiographics.11.4.1887111
B. K. Enestvedt, G. M. Eisen, J. Holub, and D. A. Lieberman, “Is the American Society of Anesthesiologists classification useful in risk stratification for endoscopic procedures?,” (in eng), Gastrointest Endosc, vol. 77, no. 3, pp. 464–471, 2013, doi: https://doi.org/10.1016/j.gie.2012.11.039
W. Kram, N. Buchholz, and O. W. Hakenberg, “Ureteral stent encrustation. Pathophysiology,” (in eng), Arch Esp Urol, vol. 69, no. 8, pp. 485–493, 2016. Incrustacion de cateteres ureterales. Fisiopatologia
M. Mitterberger, F. Frauscher, I. Steppan, R. Peschel, and G. M. Pinggera, “Ureteroiliac fistula: a case report review of the literature,” (in eng), Cases J, vol. 2, p. 6266, 2009, doi: https://doi.org/10.4076/1757-1626-2-6266
Tuite DJ, Ryan JM, Johnston C, Brophy DP, McEniff N (2006) Ureteroiliac fistula: a late sequela of radiotherapy and long-term ureteric stent placement. Clin Radiol 61(6):531–534. https://doi.org/10.1016/j.crad.2006.02.001
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was granted by the institution’s Research and Innovation Office (Ref no.: 5257).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• We describe a method for retrograde fluoroscopic exchange of ureteric double-J stents in female patients.
• We also demonstrate the flexibility and adaptability of this technique to unusual anatomy as detailed by several challenging cases.
• Retrograde ureteric stent exchange is a safe alternative to rigid cystoscopic exchange which avoids a general anaesthetic and theatre time without compromising effectiveness.
Rights and permissions
About this article
Cite this article
Smyth, R., Mulholland, D., Courtney, M. et al. Retrograde ureteric stent exchange in the female oncology patient by interventional radiology: the experience of a single tertiary referral centre. Ir J Med Sci 189, 1097–1104 (2020). https://doi.org/10.1007/s11845-020-02170-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02170-1