Abstract
Background
Peripheral arterial diseases (PAD) refer to the arterial diseases other than coronary arteries and the aorta. Atherosclerosis is the major cause of PAD. Renin angiotensin aldosterone system (RAAS)-related genes were associated with cardiovascular diseases. Angiotensin II is the pro-inflammatory, proliferative and vasoconstrictor effector of RAAS in the vascular system.
Aims
In this study, we aimed to investigate whether the effects of the angiotensinogen (AGT) rs699 (M268T), angiotensin-converting enzyme (ACE) I/D (rs1799752), angiotensin II receptor type 1 (AGTR1) (A1166C) rs5186, and angiotensin II receptor type 2 (AGTR2) rs35474657 variants were associated with PAD etiology due to atherosclerotic involvement of aorta-iliac and femoro-popliteal artery occlusions.
Methods
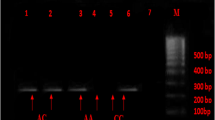
AGT rs699, AGTR1 rs5186, ACE I/D (rs1799752), AGTR2 rs35474657 gene variants were determined by real-time polymerase chain reaction (RT-PCR) in 63 PAD patients (33 femoro-popliteal, 30 aorta-iliac) and 70 healthy controls.
Results
Although there was no significant relationship in the genotype frequencies of AGT rs699, AGTR1 rs5186, ACE I/D (rs1799752), and AGTR2 rs35474657 variants between PAD and control groups (p > 0.05), AGT rs699 TT genotype was significantly associated with fasting glucose (p = 0.023) in PAD patients. Besides, CC genotype of rs699 was significantly related with HDL-cholesterol levels (p = 0.020) in PAD group. Furthermore, AGTR1 rs5186 CC genotype carriers demonstrated significantly higher LDL-cholesterol (p = 0.034) and triglycerides levels (p = 0.007).
Conclusions
This report is the first to show an association between RAAS-related gene variants and their relation with the biochemical characteristics of PAD and suggests that RAAS-associated gene variants may have significant roles in cardiovascular related phenotypes of PAD patients.

Similar content being viewed by others
References
Aboyans V, Ricco JB, MEL B et al (2018) 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Documentcovering atherosclerotic disease of extracranial carotid and vertebral,mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J 39(9):763–816
Pipinos II, Judge AR, Selsby JT, Zhu Z, Swanson SA, Nella AA, Dodd SL (2007) The myopathy of peripheral arterial occlusive disease: part 1. Functional and histomorphological changes and evidence for mitochondrial dysfunction. Vasc Endovasc Surg 41:481–489
Grenon SM, Chong K, Alley H, Nosova E, Gasper W, Hiramoto J, Boscardin WJ, Owens CD (2014) Walking disability in patients with peripheral artery disease is associated with arterial endothelial function. J Vasc Surg 59:1025–1034
Aiello A, Anichini R, Brocco E et al (2014) Treatment of peripheral arterial disease in diabetes: a consensus of the Italian societies of diabetes (SID, AMD), radiology (SIRM) and vascular endovascular surgery (SICVE). Nutr Metab Cardiovasc Dis 24(4):355–369
Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott M, Norman PE, Sampson UK, Williams LJ, Mensah GA, Criqui MH (2013) Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet 382:1329–1340
Basgoz BB, Cintosun U, Tasci İ (2017) Peripheral arterial disease and heart. Turkiye Klinikleri J Cardiol-Special Topics 10(3):173–177
Neri Serneri GG, Boddi M, Modesti PA, Coppo M, Cecioni I, Toscano T, Papa ML, Bandinelli M, Lisi GF, Chiavarelli M (2004) Cardiac angiotensin II participates in coronary microvessel inflammation of unstable angina and strengthens the immunomediated component. Circ Res 94(12):1630–1637
George AJ, Thomas WG, Hannan RD (2010) The renin-angiotensin system and cancer: old dog, new tricks. Nat Rev Cancer 10:745–759
Yin G, Yan C, Berk BC (2003) Angiotensin II signaling pathways mediated by tyrosine kinases. Int J Biochem Cell Biol 35:780–783
Sobczuk P, Szczylik C, Porta C, Czarnecka AM (2017) Renin angiotensin system deregulation as renal cancer risk factor. Oncol Lett 14(5):5059–5068
Brand E, Chatelain N, Paillard F, Tiret L, Visvikis S, Lathrop M, Soubrier F, Demenais F (2002) Detection of putative functional angiotensinogen (AGT) gene variants controlling plasma AGT levels by combined segregation-linkage analysis. Eur J Hum Genet 10(11):715–723
Sethi AA, Nordestgaard BG, Tybjaerg-Hansen A (2003) Angiotensinogen gene polymorphism, plasma angiotensinogen, and risk of hypertension and ischemic heart disease: a meta-analysis. Arterioscler Thromb Vasc Biol 23(7):1269–1275
World Health Organization (1999) Definition, diagnosis and classification of diabetes mellitus and its complications. Report of a WHO Consult. Part 1: Diagnosis and Classification of Diabetes Mellitus. Geneva: WHO Department of Noncommunicable Disease Surveillance:1–59
https://www.omim.org/entry/106180. Last accessed 17-July-2019
Rigat B, Hubert C, Alhenc-Gelas F, Cambien F, Corvol P, Soubrier F (1990) An insertion/ deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Invest 86:1343–1346
Wang WY, Zee RY, Morris BJ (1997) Association of angiotensin II type 1 receptor gene polymorphism with essential hypertension. Clin Genet 51(1):31–34
Parchwani DN, Patel DD, Rawtani J, Yadav D (2018) Analysis of association of angiotensin II type 1 receptor gene A1166C gene polymorphism with essential hypertension. Indian J Clin Biochem 33(1):53–60
Jiang Z, Zhao W, Yu F, Xu G (2001) Association of angiotensin II type 1 receptor gene polymorphism with essential hypertension. Chin Med J 114(12):1249–1251
Ono K, Mannami T, Baba S et al (2003) Lack of association between angiotensin II type 1 receptor gene polymorphism and hypertension in Japanese. Hypertens Res 26(2):131–134
Han W, Sun N, Chen L et al (2017) Relationship of renin-angiotensin system polymorphisms with ambulatory and central blood pressure in patients with hypertension. J Clin Hypertens (Greenwich) 19(11):1081–1087
Hein L, Barsh GS, Pratt RE et al (1995) Behavioural and cardiovascular effects of disrupting the angiotensin II type-2 receptor in mice. Nature 377(6551):744–747 Erratum in: nature 1996 mar 28;380(6572):366
Schütz S, Le Moullec JM, Corvol P et al (1996) Early expression of all the components of the renin-angiotensin-system in human development. Am J Pathol 149:2067–2079
Nishimura H, Yerkes E, Hohenfellner K, Miyazaki Y, Ma J, Hunley TE, Yoshida H, Ichiki T, Threadgill D, Phillips JA 3rd, Hogan BM, Fogo A, Brock JW 3rd, Inagami T, Ichikawa I (1999) Role of the angiotensin type 2 receptor gene in congenital anomalies of the kidney and urinary tract, CAKUT, of mice and men. Mol Cell 3(1):1–10
Vervoort VS, Beachem MA, Edwards PS, Ladd S, Miller KE, de Mollerat X, Clarkson K, DuPont B, Schwartz CE, Stevenson RE, Boyd E, Srivastava AK (2002) AGTR2 mutations in X-linked mental retardation. Science 296(5577):2401–2403
Piton A, Redin C, Mandel JL (2013) XLID-causing mutations and associated genes challenged in light of data from large-scale human exome sequencing. Am J Hum Genet 93(2):368–383 Erratum in: Am J Hum Genet 2013 Aug 8;93(2):406
Miranda DM, Dos Santos AC Jr, Sarubi HC et al (2014) Association of angiotensin type 2 receptor gene polymorphisms with ureteropelvic junction obstruction in Brazilian patients. Nephrology (Carlton) 19(11):714–720
Deser SB, Bayoglu B, Besirli K, Cengiz M, Arapi B, Junusbekov Y, Dirican A, Arslan C (2016) Increased IL18 mRNA levels in peripheral artery disease and its association with triglyceride and LDL cholesterol levels: a pilot study. Heart Vessel 31(6):976–984
Hiatt WR (2001) Medical treatment of peripheral arterial disease and claudication. N Engl J Med 344:1608–1621
Abd El-Aziz TA, Hussein YM, Mohamed RH et al (2012) Renin-angiotensin system genes polymorphism in Egyptians with premature coronary artery disease. Gene 498(2):270–275
Jia EZ, Xu ZX, Guo CY, Li L, Gu Y, Zhu TB, Wang LS, Cao KJ, Ma WZ, Yang ZJ (2012) Renin-angiotensin-aldosterone system gene polymorphisms and coronary artery disease: detection of gene-gene and gene-environment interactions. Cell Physiol Biochem 29(3–4):443–452
Xia MM, Wang M, Jiang H, Liu Y, Ma L, Lu C, Zhang W (2019) Association of angiotensin-converting enzyme insertion/deletion polymorphism with the risk of atherosclerosis. J Stroke Cerebrovasc Dis 28(6):1732–1743
Jeunemaitre X, Soubrier F, Kotelevtsev YV, Lifton RP, Williams CS, Charru A, Hunt SC, Hopkins PN, Williams RR, Lalouel JM (1992) Molecular basis of human hypertension: role of angiotensinogen. Cell 71(1):169–180
Su X, Lee L, Li X, Lv J, Hu Y, Zhan S, Cao W, Mei L, Tang YM, Wang D, Krauss RM, Taylor KD, Rotter JI, Yang H (2007) Association between angiotensinogen, angiotensin II receptor genes, and blood pressure response to an angiotensin-converting enzyme inhibitor. Circulation 115(6):725–732
Imbalzano E, Vatrano M, Quartuccio S, di Stefano R, Aragona CO, Mamone F, D'Ascola A, Scuruchi M, Felice F, Trapani G, Alibrandi A, Ciconte VA, Ceravolo R, Saitta A, Mandraffino G (2017) Clinical impact of angiotensin I converting enzyme polymorphisms in subjects with resistant hypertension. Mol Cell Biochem 430(1–2):91–98
Yang Y, Tian T, Lu J, He H, Xing K, Tian G (2017) A1166C polymorphism of the angiotensin II type 1 receptor gene contributes to hypertension susceptibility: evidence from a meta-analysis. Acta Cardiol 72(2):205–215. https://doi.org/10.1080/00015385.2017.1291211
Taute BM, Handschug K, Taute R, Seifert H, Gläser C, Podhaisky H (1998) Angiotensin-converting enzyme gene insertion/deletion polymorphism and peripheral arterial occlusive disease. Vasa 27(3):149–153
Taute BM, Gläser C, Taute R, Podhaisky H (2002) Progression of atherosclerosis in patients with peripheral arterial disease as a function of angiotensin-converting enzyme gene insertion/deletion polymorphism. Angiology 53(4):375–382
Li R, Nicklas B, Pahor M, Newman A, Sutton-Tyrrell K, Harris T, Lakatta E, Bauer DC, Ding J, Satterfield S, Kritchevsky SB (2007) Polymorphisms of angiotensinogen and angiotensin-converting enzyme associated with lower extremity arterial disease in the health, aging and body composition study. J Hum Hypertens 21(8):673–682
Fatini C, Sticchi E, Sofi F, Said AA, Pratesi G, Pulli R, Pratesi C, Abbate R (2009) Multilocus analysis in candidate genes ACE, AGT, and AGTR1 and predisposition to peripheral arterial disease: role of ACE D/−240T haplotype. J Vasc Surg 50(6):1399–1404
Scicchitano P, Cameli M, Maiello M et al (2014) Nutraceuticals and dyslipidaemia: beyond the common therapeutics. J Funct Foods 6:11–32
Paulis L, Foulquier S, Namsolleck P, Recarti C, Steckelings UM, Unger T (2016) Combined angiotensin receptor modulation in the management of cardio-metabolic disorders. Drugs 76(1):1–12
Barrons RW, Woods JA (2016) The roles of ACE inhibitors in lower extremity peripheral artery disease. Am J Ther 23(1):e7–e15
Acknowledgments
The findings of this study were presented at the VII. International Congress of Molecular Medicine, Istanbul, Turkey, September 5-7, 2019.
Funding
This study was partly funded by the Scientific Research Projects Coordination Unit of Istanbul University-Cerrahpasa (grant number 34151).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Junusbekov, Y., Bayoglu, B., Cengiz, M. et al. AGT rs699 and AGTR1 rs5186 gene variants are associated with cardiovascular-related phenotypes in atherosclerotic peripheral arterial obstructive disease. Ir J Med Sci 189, 885–894 (2020). https://doi.org/10.1007/s11845-019-02166-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02166-6