Abstract
Background and aims
Urosepsis accounts for up to 20–30% of all sepsis cases; however, increasing antimicrobial resistance is posing a significant threat to patient’s outcomes. The aim of this study was to look at the prevalence of multi-drug resistant (MDR) organisms in patients admitted with urosepsis and their effect on the treatment and outcome of patients in our hospital.
Methods
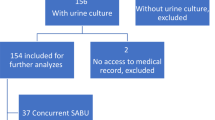
A total of 2679 urine cultures and 654 blood cultures performed in Connolly Hospital Emergency Department were reviewed between 2016 and 2018. Patients were included if they had a matching urine culture and blood culture performed within 24 h of admission. We compared patient demographics and underlying co-morbidities between patients admitted with urosepsis secondary to MDR organisms and non-MDR organisms.
Results
Our study included 85 patients admitted with urosepsis. The most common causative pathogen was Escherichia coli, and 34.1% (n = 29) of pathogens were classified as an MDR organism. Patients admitted with urosepsis from long-term care facilities were 2.3 times more likely to have urosepsis due to a MDR organism compared with patients admitted from the community. Patients admitted with urosepsis secondary to a MDR organism were also more likely to have co-morbidities such as diabetes and dementia.
Conclusion
The high rate of antimicrobial resistance in patients admitted with urosepsis poses a challenge in prescribing the most appropriate antibiotics. It is crucial that prescribers follow local antibiotic guidelines for the treatment of urosepsis and are cognisant of the risk of specific patient groups presenting with urosepsis due to MDR organisms.


Similar content being viewed by others
References
Dreger NM, Degener S, Ahmad-Nejad P, Wobker G, Roth S (2015) Urosepsis--etiology, diagnosis, and treatment. Dtsch Arztebl Int 112(49):837–847 quiz 848
Peach BC, Garvan GJ, Garvan CS, Cimiotti JP (2016) Risk factors for urosepsis in older adults: a systematic review. Gerontol Geriatr Med 2:2333721416638980
Spellberg B, Blaser M, Guidos RJ, Boucher HW, Bradley JS, Eisenstein BI et al (2011) Combating antimicrobial resistance: policy recommendations to save lives. Clin Infect Dis 52(Suppl 5):S397–S428
Department of Health (2017) Ireland’s national action plan on antimicrobial resistance 2017-2020. iNAP, Dublin
Vardakas KZ, Rafailidis PI, Konstantelias AA, Falagas ME (2013) Predictors of mortality in patients with infections due to multi-drug resistant Gram negative bacteria: the study, the patient, the bug or the drug? J Inf Secur 66(5):401–414
van Duin D, Paterson DL (2016) Multidrug-resistant bacteria in the community: trends and lessons learned. Infect Dis Clin N Am [Internet] 30(2):377–390 Available from: https://www.ncbi.nlm.nih.gov/pubmed/27208764
Associated TRC of PCAG on H. Guidelines for the prevention and control of multi-drug resistant organisms (MDRO) excluding MRSA in the healthcare setting. [Internet]. Dublin; 2014. Available from: http://hdl.handle.net/10147/303397. Accessed August 2019
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA [Internet] 315(8):801–810 Available from: https://www.ncbi.nlm.nih.gov/pubmed/26903338
EARS-Net Report 2011, on Health Services Executive (HSE) - Health protection surveillance centre (HPSC) [Internet]. 2011. Available from: https://ecdc.europa.eu/en/publications-data/antimicrobial-resistance-surveillance-europe-2011. Accessed August 2019
Ben-Ami R, Rodriguez-Bano J, Arslan H, Pitout JDD, Quentin C, Calbo ES et al (2009) A multinational survey of risk factors for infection with extended-spectrum beta-lactamase-producing enterobacteriaceae in nonhospitalized patients. Clin Infect Dis 49(5):682–690
Huang Y-WY, Alleyne A, Leung V, Chapman M (2018) Urosepsis due to extended-spectrum beta-lactamase-producing Escherichia coli: a retrospective, single-centre review of risk factors and clinical outcomes. Can J Hosp Pharm 71(2):119–127
Martin GS, Mannino DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 348(16):1546–1554
Rosenthal EJK (2002) Epidemiology of septicaemia pathogens. Dtsch Med Wochenschr 127(46):2435–2440
Wagenlehner FME, Pilatz A, Weidner W, Naber KG (2015) Urosepsis: Overview of the diagnostic and treatment challenges. Microbiol Spectr 3(5)
Acknowledgments
We would like to acknowledge Anne Maclellan and Grainne Bowens, Surveillance Scientists, Connolly Hospital for their assistance in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ryan, J., McLornan, L. & O’Neill, E. The impact of increasing antimicrobial resistance in the treatment of urosepsis. Ir J Med Sci 189, 611–615 (2020). https://doi.org/10.1007/s11845-019-02118-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02118-0