Abstract
Background
The prognosis for patients with liver metastases from gastric cancer is very poor. Nevertheless, standard therapeutic strategies have not been established yet. The impact of hepatic surgical treatment on survival of patients with metachronous liver metastases from gastric cancer still remains controversial.
Methods
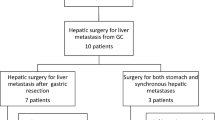
We conducted a retrospective analysis on records of 436 patients who received radical gastrectomy (with D2 lymphadenectomy, regardless of hepatic surgical treatment) for gastric cancer with metachronous (≥ 3 months after gastrectomy) liver metastases in our center between 2001 and 2016. All patients were followed until 2017/10/31 or withdrawn from the follow-up because of death.
Results
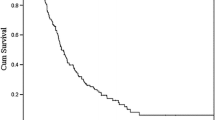
The median interval for non-hepatic metastases of the 436 patients who underwent radical gastrectomy is 14 months. T (P = 0.041), N (P = 0.023) and lymphovascular invasion (P < 0.001) were independent predictors affecting liver metastases-free interval. The overall survival rates for the 436 patients were 44.5, 29.7, 16.3, and 16.3% at 1, 2, 3, and 5 years respectively since treatment of hepatic metastases, with a median survival time of 11 months. N (P = 0.025), extent of liver metastases (H) (H2 vs. H1, P = 0.036; H3 vs. H1, P < 0.001), and treatment of liver metastatic lesions (P < 0.001) were significant independent prognostic factors for survival after presence of liver metastases. Among H1 and H2 patients, median survival in hepatic surgical treatment group was significantly longer than that in systemic chemotherapy alone group (25 vs. 11 months, P = 0.015).
Conclusions
Liver examinations should be performed during the first 2 years after gastric surgery and continued for 5 years for high-risk patients. Active therapeutic strategies may prolong patients’ survival compared with supportive treatment alone. Patients with H1, H2 metachronous liver metastases may be considered appropriate candidates for hepatic surgical treatment before embarking on systemic chemotherapy alone.
Trial registration
ISRCTN Registry (Retrospectively registered; Reference number: 35067; Date: 02/04/2018).






Similar content being viewed by others
Abbreviations
- GC:
-
gastric carcinoma
- GCCM:
-
colorectal metastases from gastric cancer
- GCMLM:
-
gastric cancer with metachronous liver metastases
- GCLM:
-
liver metastases from gastric cancer
- TACE:
-
transcatheter arterial chemoembolization
- MCT:
-
microwave coagulation therapy
- MST:
-
median survival time
References
Thun MJ, DeLancey JO, Center MM, Center MM, Jemal A, Ward EM (2010) The global burden of cancer: priorities for prevention. Carcinogenesis 31:100–110
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Blot WJ, Devesa SS, Kneller RW, Fraumeni JF Jr (1991) Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA 265:1287–1289
Kamangar F, Dores GM, Anderson WF (2006) Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol 24:2137–2150
D’Angelica M, Gonen M, Brennan MF, Turnbull AD, Bains M, Karpeh MS (2004) Patterns of initial recurrence in completely resected gastric adenocarcinoma. Ann Surg 240:808–816
Sakamoto Y, Sano T, Shimada K, Esaki M, Saka M, Fukagawa T et al (2007) Favorable indications for hepatectomy in patients with liver metastasis from gastric cancer. J Surg Oncol 95:534–539
Tiberio GA, Coniglio A, Marchet A, Marrelli D, Giacopuzzi S, Baiocchi L et al (2009) Metachronous hepatic metastases from gastric carcinoma: a multicentric survey. Eur J Surg Oncol 35:486–491
Slupski M, Wlodarczyk Z, Jasinski M, Masztalerz M, Tujakowski J (2009) Outcomes of simultaneous and delayed resections of synchronous colorectal liver metastases. Can J Surg 52:E241–E244
Saiura A, Umekita N, Inoue S, Maeshiro T, Miyamoto S, Matsui Y et al (2002) Clinicopathological features and outcome of hepatic resection for liver metastasis from gastric cancer. Hepato-Gastroenterology 49:1062–1065
Kunisaki C, Makino H, Takagawa R, Oshima T, Nagano Y, Fujii S et al (2008) Impact of palliative gastrectomy in patients with incurable advanced gastric cancer. Anticancer Res 28:1309–1315
Cheon SH, Rha SY, Jeung HC, Im CK, Kim SH, Kim HR et al (2008) Survival benefit of combined curative resection of the stomach (D2 resection) and liver in gastric cancer patients with liver metastases. Ann Oncol 19:1146–I 153
Sakamoto Y, Ohyama S, Yamamoto J, Yamaka K, Seki M, Ohta K et al (2003) Surgical resection of liver metastases of gastric cancer: an analysis of a 17-year experience with 22 patients. Surgery 133:507–511
Ajani JA (2005) Evolving chemotherapy for advanced gastric cancer. Oncologist 10(Suppl 3):49–58
Shin A, Kim J, Park S (2011) Gastric cancer epidemiology in Korea. J Gastric Cancer 11:135–140
Li C, Yan M, Chen J, Xiang M, Zhu ZG, Yin HR et al (2010) Survival benefit of non-curative gastrectomy for gastric cancer patients with synchronous distant metastasis. J Gastrointest Surg 14:282–288
Zacherl J, Zacherl M, Scheuba C, Steininger R, Wenzl E, Mühlbacher F et al (2002) Analysis of hepatic resection of metastasis originating from gastric adenocarcinoma. J Gastrointest Surg 6:682–689
Markar SR, Mikhail S, Malietzis G, Athanasiou T, Mariette C, Sasako M et al (2016) Influence of surgical resection of hepatic metastases from gastric adenocarcinoma on long-term survival: systematic review and pooled analysis. Ann Surg 263:1092–1101
Tsujimoto H, Ichikura T, Ono S, Suqasawa H, Hiraki S, Sakamoto N et al (2010) Outcomes for patients following hepatic resection of metastatic tumors from gastric cancer. Hepatol Int 4:406–413
Marrelli D, Roviello F, De Stefano A, Fotia G, Giliberto C, Garosi L et al (2004) Risk factors for liver metastases after curative surgical procedures for gastric cancer: a prospective study of 208 patients treated with surgical resection. J Am Coll Surg 198:51–58
Takemura N, Saiura A, Koga R, Arita J, Yoshioka R, Ono Y et al (2012) Long-term outcomes after surgical resection for gastric cancer liver metastasis: an analysis of 64 macroscopically complete resections. Langenbeck's Arch Surg 397:951–957
Kumagai K, Tanaka T, Yamagata K, Yokoyama N, Shimizu K (2001) Liver metastasis in gastric cancer with particular reference to lymphatic advancement. Gastric Cancer 4:150–155
Koga S, Takebayashi M, Kaibara N, Nishidoi H, Kimura O, Kawasumi H et al (1987) Pathological characteristics of gastric cancer that develop hematogenous recurrence, with special reference to the site of recurrence. J Surg Oncol 36:239–242
Maehara Y, Orita H, Okuyama T, Moriguchi S, Tsujitani S, Korenaga D et al (1992) Predictors of lymph node metastasis in early gastric cancer. Br J Surg 79:245–247
Saito H, Tsujitani S, Kondo A, Ikeguchi M, Maeta M, Kaibara N (1999) Expression of vascular endothelial growth factor correlates with hematogenous recurrence in gastric carcinoma. Surgery 125:195–201
Hyung WJ, Lee JH, Choi SH, Min JS, Noh SH (2002) Prognostic impact of lymphatic and/or blood vessel invasion in patients with node-negative advanced gastric cancer. Ann Surg Oncol 9:562–567
Dicken BJ, Graham K, Hamilton SM, Andrews S, Lai R, Listgarten J (2006) Lymphovascular invasion is associated with poor survival in gastric cancer: an application of gene-expression and tissue array techniques. Ann Surg 243:64–73
Okano K, Maeba T, Ishimura K, Karasawa Y, Goda F, Wakabayashi H et al (2002) Hepatic resection for metastatic tumors from gastric cancer. Ann Surg 235:86–91
Kwok CM, Wu CW, Lo SS, Shen KH, Hsieh MC, Lui WY (2004) Survival of gastric cancer with concomitant liver metastases. Hepato-Gastroenterology 51:1527–1530
Lim S, Muhs BE, Marcus SG, Newman E, Berman RS, Hiotis SP (2007) Results following resection for stage IV gastric cancer; are better outcomes observed in selected patient subgroups? J Surg Oncol 95:118–122
Ueda K, Iwahashi M, Nakamori M, Nakamura M, Naka T, Ishida K et al (2009) Analysis of the prognostic factors and evaluation of surgical treatment for synchronous liver metastases from gastric cancer. Langenbeck's Arch Surg 394:647–653
Saito H, Yamada Y, Tsujitani S, Ikequchi M (2009) Clinicopathologic characteristics of gastric cancer patients who underwent noncurative gastrectomy with long-term survival. Langenbeck's Arch Surg 394:99–103
Morise Z, Sugioka A, Hoshimoto S, Kato T, Ikeda M, Uyama I et al (2008) The role of hepatectomy for patients with liver metastases of gastric cancer. Hepato-Gastroenterology 55:1238–1241
Leong T (2005) Chemotherapy and radiotherapy in the management of gastric cancer. Curr Opin Gastroenterol 21:673–678
Samarasam I, Chandran BS, Sitaram V, Perakath B, Nair A, Mathew G (2006) Palliative gastrectomy in advanced gastric cancer: is it worthwhile? ANZ J Surg 76:60–63
Koga R, Yamamoto J, Ohyama S, Saiura A, Seki M, Seto Y et al (2007) Liver resection for metastatic gastric cancer: experience with 42 patients including eight long-term survivors. Jpn J Clin Oncol 37:836–842
Miyagaki H, Fujitani K, Tsujinaka T, Hirao M, Yasui M, Kashiwazaki M et al (2008) The significance of gastrectomy in advanced gastric cancer patients with non-curative factors. Anticancer Res 28:2379–2384
Hwang SE, Yang DH, Kim CY (2009) Prognostic factors for survival in patients with hepatic recurrence after curative resection of gastric cancer. World J Surg 33:1468–1472
Hirasawa T, Asahara S, Fujisaki S, Kuraoka K, Takano K, Kamei A et al (2008) Transcatheter arterial chemoembolization (TACE) using degradable starch microspheres (DSM) for metastatic liver tumors in patients with gastric cancer. Nippon Shokakibyo Gakkai Zasshi 105:367–372
Acknowledgements
The authors are grateful to all doctors at the relevant departments for their clinical practice on the enrolled patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Yibin Xiao designed the research; Yibin Xiao, Bo Zhang, and Yulian Wu collected and analyzed the data; Yibin Xiao wrote and revised the manuscript; Yulian Wu provided analytic tools and checked the accuracy of the data. All the authors approved the version to be published.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was reviewed and approved by the ethical committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University. All patients were followed up by phone call or SMS and explained clearly that data collected will be intended for publication. All methods were performed in accordance with the relevant guidelines and regulations.
Competing interests
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Xiao, Y., Zhang, B. & Wu, Y. Prognostic analysis and liver metastases relevant factors after gastric and hepatic surgical treatment in gastric cancer patients with metachronous liver metastases: a population-based study. Ir J Med Sci 188, 415–424 (2019). https://doi.org/10.1007/s11845-018-1864-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1864-4