Abstract
Background
Acute optic neuritis (ON) is often the first manifestation of multiple sclerosis which is particularly common in Ireland. Despite the specific clinical details regarding investigations and management of ON provided by the Optic Neuritis Treatment Trial (ONTT), international surveys have shown that there are still notable differences in the management of ON between neurologists and ophthalmologists.
Aim
To compare the investigation and treatment of acute optic neuritis between ophthalmologists and neurologists in Ireland
Method
A survey consisting of a case scenario and questions regarding treatment and investigations of a patient with ON was emailed to ophthalmology consultants, trainees and medical ophthalmologists registered with the Irish College of Ophthalmologists and to neurology consultants and registrars registered with the Irish Institute of Clinical Neuroscience.
Results
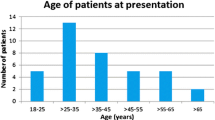
One hundred sixty recipients responded out of 350 (46%). The majority of the neurologists would initiate steroid treatment regardless of the patient’s vision (75%), treat with 1 g IV methylprednisolone (100%) for 5 days (57%), perform an MRI brain and orbits with contrast (92%) and multiple laboratory tests (96%). In contrast, the ophthalmologists tended to initiate treatment depending on the patient’s vision (48%), treat with 1 g IV methylprednisolone (97%) for 3 days instead of 5 days (93%), perform MRI brain and orbits with contrast (73%) and favour electrophysiology testing (73%) over laboratory testing (68%).
Conclusions
Overall, most respondents would follow the ONTT guidelines regarding IV methylprednisolone. There was a significant difference in responses between the ophthalmologists and neurologists regarding who to treat, duration of treatment and appropriate investigations.


Similar content being viewed by others
References
Lonergan R, Kinsella K, Fitzpatrick P, Brady J, Murray B, Dunne C, Hagan R, Duggan M, Jordan S, McKenna M, Hutchinson M, Tubridy N (2011) Multiple sclerosis prevalence in Ireland: relationship to vitamin D status and HLA genotype. J Neurol Neurosurg Psychiatry 82(3):317–322. https://doi.org/10.1136/jnnp.2010.220988
McGuigan C, McCarthy A, Quigley C, Bannan L, Hawkins SA, Hutchinson M (2004) Latitudinal variation in the prevalence of multiple sclerosis in Ireland, an effect of genetic diversity. J Neurol Neurosurg Psychiatry 75(4):527–576. https://doi.org/10.1136/jnnp.2003.012666
Beck RW, Gal RL (2008) Treatment of acute optic neuritis: a summary of findings from the optic neuritis treatment trial. Arch Ophthalmol 126(7):994–995. https://doi.org/10.1001/archopht.126.7.994
Brodsky M, Nazarian S, Orengo-Nania S et al (2008) The Optic Neuritis Study Group. Multiple sclerosis risk after optic neuritis: final optic neuritis treatment follow-up. Arch Neurol 65(6):727–732. https://doi.org/10.1001/archneur.65.6.727
Beck RW, Cleary PA, Trobe JD, Kaufman DI, Kupersmith MJ, Paty DW, Brown CH (1993) The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. N Engl J Med 329:1764–1769. https://doi.org/10.1056/NEJM/1993120932922403
Beck RW, Arrington J, Reed Murtagh F et al (1993) Brain magnetic resonance imaging in acute optic neuritis. Arch Neurol 50(8):841–846. https://doi.org/10.1001/archneur.1993.00540080050013
Beck RW, Cleary PA, Backlund J et al (1994) The course of visual recovery after optic neuritis. Ophthalmology 101:1771–1778. https://doi.org/10.1016/S0161-6420(94)31103-1
Ghosh A, Kelly SP, Mathews J, Cooper PN, Macdermott N (2002) Evaluation of the management of optic neuritis: audit on the neurological and ophthalmological practice in the north west of England. J Neurol Neurosurg Psychiatry 71:119–121. https://doi.org/10.1136/jnnp.72.1.119
Biousse V, Calvetti O, Drews-Botsch CD, Atkins EJ, Sathornsumetee B, Newman NJ, Optic Neuritis Survey Group (2009) Management of optic neuritis and impact of clinical trials: an international survey. J Neurol Sci 275(1–2):69–74. https://doi.org/10.1016/j.jns.2008.08.039
Atkins EJ, Drews-Botsch CD, Newman NJ, Calvetti O, Swanson S, Biousse V (2008) Management of optic neuritis in Canada: survey of ophthalmologists and neurologists. Can J Neurol Sci 35(2):179–184. https://doi.org/10.1017/S031716710000860X
Lueck CJ, Danesh-Meyer HV, Margrie FJ, Drews-Botsch C, Calvetti O, Newman NJ, Biousse V (2008) Management of acute optic neuritis: a survey of ophthalmologists and neurologists in Australia and New Zealand. J Clin Neurosci 15(3):1340–1345. https://doi.org/10.1016/j.jocn.2008.01.014
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study and identifiable data remained anonymous throughout the study.
Appendix
Appendix
Questionnaire
A 25 year old Irish Caucasian female presents with acute unilateral loss of vision with pain on eye movements. She has no previous ophthalmic history or medical history and is on no medication. You make the diagnosis of a first episode of Acute Retrobulbar Optic Neuritis.
Please answer the following questions regarding the treatment of this patient
-
1)
At what visual acuity would you initiate steroids in this patient?
-
○ Better than 6/24
-
○ 6/24 – 6/60
-
○ Less than 6/60
-
○ I would initiate steroid treatment regardless of the visual acuity
-
○ I would not initiate steroid treatment for this patient
-
-
2)
Would you routinely:
-
○ Treat as an inpatient
-
○ Day services administration of treatment as an outpatient
-
○ Treat solely as an outpatient
-
-
3)
What would be your preferred route and dose of initial steroid therapy?
-
○ 1g IV Methylprednisolone
-
○ 1mg/kg per os prednisolone
-
○ No steroid treatment
-
○ Other steroid regime (please specify)
-
-
4)
Initial steroid treatment routinely given for:
-
○ 3 days
-
○ 5 days
-
○ More than 5 days
-
-
5)
Your preferred dosing schedule for IVI Methylprednisolone:
-
○ Once daily
-
○ 500mg 12 hourly
-
○ 250mg 6 hourly
-
-
6)
Regarding per os steroid following initial treatment:
-
○ Taper to a complete stop in 11 days
-
○ Continue 1mg/kg po prednisolone for 11 days then taper
-
○ No per os steroid after initial treatment
-
○ Other (please specify)
-
-
7)
Would you prescribe gastric protection?
-
○ Yes
-
○ No
-
-
8)
Would you prescribe calcium supplements?
-
○ Yes
-
○ No
-
-
9)
Which radiological investigations would you routinely order for this case? (multiple options allowed)
-
○ CT brain and orbits
-
○ CT brain and orbits with contrast
-
○ MRI brain and orbits
-
○ MRI brain and orbits with contrast
-
○ Chest Xray
-
○ None
-
-
10)
Which laboratory investigations would you routinely order for this case? (multiple options allowed)
-
○ Lumbar puncture
-
○ Full blood count
-
○ Urea and electrolytes
-
○ ESR and CRP
-
○ Syphillis serology
-
○ Thyroid function tests
-
○ Borrelia burgdorferi
-
○ HSV
-
○ TB
-
○ HIV
-
○ Autoimmune screen
-
○ NMO antibody
-
○ None
-
-
11)
Regarding electrophysiology and field testing, which would you routinely order for this case?
-
○ Visual evoked potential (VEP)
-
○ Electroretinogram (ERG)
-
○ Humphrey visual fields (HVF)
-
○ Goldmann perimetry
-
○ None
-
-
12)
Would you mention the possible diagnosis of Multiple Sclerosis to the patient?
-
○ Yes
-
○ No
-
-
13)
What is your current professional status?
-
○ Consultant Neurologist
-
○ Neurology trainee
-
○ Consultant Ophthalmologist
-
○ Medical Ophthalmologist
-
○ Ophthalmology trainee
-
-
14)
Would you treat this patient?
-
○ Yes, I would treat this patient
-
○ Yes, I would treat this patient but request an opinion from a Neuro-Ophthalmologist
-
○ Yes, I would treat this patient but request an opinion from a Neurologist
-
○ Yes, I would treat this patient but request an opinion from a Neuro-Ophthalmologist and a Neurologist
-
○ Yes, but under supervision as I am a trainee
-
○ No, I would refer to a Neuro-Ophthalmologist
-
○ No, I would refer to a Neurologist
-
○ No, I would refer to a Neuro-Ophthalmologist and a Neurologist
-
Note: respondents that selected ‘I would not initiate steroid treatment for this patient’ for the first questions were allowed to skip to the investigations section (question 9) of the questionnaire.
Rights and permissions
About this article
Cite this article
Kobayter, L., Chetty, S. Management of optic neuritis in Ireland: a survey comparing the management practices of acute demyelinating optic neuritis amongst ophthalmologists and neurologists in Ireland. Ir J Med Sci 188, 277–282 (2019). https://doi.org/10.1007/s11845-018-1817-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1817-y