Abstract
Background
Hypertensive urgency is defined as a severely elevated systolic blood pressure (SBP) of ≥ 180 mmHg and/or diastolic blood pressure (DBP) of ≥ 120 mmHg, in the absence of end organ damage. It is known that there are racial differences in prevalence and severity of hypertension but there is a dearth of studies looking at hypertensive urgency in Black populations living in Europe.
Aims
We sought to define the clinical characteristics of Black patients presenting with hypertensive urgency, in order to better define the risks and complications this growing population of patients faces.
Methods
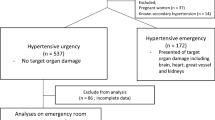
This was a single-centre retrospective cohort study of 63 consecutive Black and Afro-Caribbean patients attending a South London district general hospital outpatient hypertension clinic from April 2014 to June 2016. All patients had initially presented with hypertensive urgency to their GP, the Emergency Department, or the hospital’s medical take.
Results
The cohort had a mean age of 52.7 years and an even gender balance. Thirty-four patients had a pre-existing diagnosis of hypertension, with a 9-year median time since diagnosis. This was the first presentation of hypertension for the remaining 46%. Other comorbidities found were diabetes mellitus (10%), ischaemic heart disease (5%), hyperlipidaemia (5%), and cerebrovascular disease (2%). Patients who drank alcohol regularly were found to have significantly higher blood pressures than those who did not. Most patients presented with typical symptoms of uncontrolled hypertension, with headache (25%) and chest pain (16%) being most common. Features of end organ damage were also common, with 32 patients having hypertensive retinopathy, 16 patients having proteinuria and 14 patients found to have left ventricular hypertrophy on echocardiography.
Conclusion
The large proportion of newly diagnosed hypertensive patients presenting with end organ signs of prolonged uncontrolled hypertension suggests that there are significant numbers of undiagnosed Black patients in the community, suggesting that we should more actively conduct test for hypertension and its complications when we encounter these patients, who constitute a growing part of the populations in Europe.
Similar content being viewed by others
References
SERVICES USDOHAH. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. In: Health NIo, National Heart L, and Blood Institute, Program NHBPE, eds. United States of America: U.S. Department Of Health and Human Services 2004:54
Bender SR, Fong MW, Heitz S, Bisognano JD. Characteristics and management of patients presenting to the emergency department with hypertensive urgency. Journal of clinical hypertension. 8(1):12–18
Borzecki AM, Kader B, Berlowitz DR (2010) The epidemiology and management of severe hypertension. J Hum Hypertens 24(1):9–18
Zampaglione B, Pascale C, Marchisio M, Cavallo-Perin P (1996) Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension 27(1):144–147
Jay SJ (1998) Cigarette smoking and severe uncontrolled hypertension in inner-city African Americans. Am J Med 105(1):83–84
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA.303(20):2043–2050
Bosworth HB, Dudley T, Olsen MK, et al. Racial differences in blood pressure control: potential explanatory factors. The American journal of medicine. 2006;119(1):70 e79–15
Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH, Hall WD, Jones WE, Kountz DS, Lea JP, Nasser S, Nesbitt SD, Saunders E, Scisney-Matlock M, Jamerson KA, on behalf of the International Society on Hypertension in Blacks (2010) Management of high blood pressure in Blacks: an update of the international society on hypertension in Blacks consensus statement. Hypertension 56(5):780–800
Shea S, Misra D, Ehrlich MH, Field L, Francis CK (1992) Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. N Engl J Med 327(11):776–781
Excellence NIoC. Hypertension in adults: diagnosis and management-guideline. In: Excellence NIoC, ed. United Kingdom: National Institute of Clinical Excellence 2011:9
Vilela-Martin JF, Vaz-de-Melo RO, Kuniyoshi CH, Abdo AN, Yugar-Toledo JC (2011) Hypertensive crisis: clinical-epidemiological profile. Hypertens Res 34(3):367–371
Vlcek M, Bur A, Woisetschläger C, Herkner H, Laggner AN, Hirschl MM (2008) Association between hypertensive urgencies and subsequent cardiovascular events in patients with hypertension. J Hypertens 26(4):657–662
Caligiuri SP, Austria JA, Pierce GN (2017) Alarming prevalence of emergency hypertension levels in the general public identified by a hypertension awareness campaign. Am J Hypertens:hpw136
Windsor-Shellard B. Adult drinking habits in Great Britain - Office for National Statistics [Internet]. Ons.gov.uk. 2018 [cited 1 March 2018]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/drugusealcoholandsmoking/bulletins/opinionsandlifestylesurveyadultdrinkinghabitsingreatbritain/2005to2016
Richardson SI, Freedman BI, Ellison DH, Rodriguez CJ (2013) Salt sensitivity: a review with a focus on non-Hispanic blacks and Hispanics. J Am Soc Hypertens 7(2):170–179
Cherney D, Straus S (2002) Management of patients with hypertensive urgencies and emergencies: a systematic review of the literature. J Gen Intern Med 17(12):937–945
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Statement of authorship
The authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Rights and permissions
About this article
Cite this article
Maweni, R.M., Sunderland, N., Rahim, Z. et al. Clinical characteristics of Black patients with hypertensive urgency. Ir J Med Sci 187, 1089–1096 (2018). https://doi.org/10.1007/s11845-018-1787-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1787-0