Abstract
Introduction
Clinical handover is defined as inter-clinician communication occurring at care interfaces. In this study, we analyse the clinical outcomes and physician attitudes associated with the implementation of a electronic clinical handover system in our medical department.
Aim
The aim of this project was to introduce a reliable, standardised, reproducible method of communicating information regarding inpatients within our medical department. We also sought to assess the attitudes of physicians within our department to medical handover.
Methods
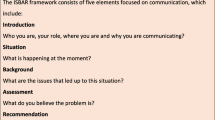
We designed and implemented an electronic handover template with a protocol to guide staff as to its use. Handover was audited weekly. In addition, we surveyed attitudes of doctors to handover before and after our handover pilot.
Results
An average of 32 patients were handed over each week. Compliance with mandatory handover of ICU/CCU patients averaged at 59%. Extrapolating our pilot results for the year would result in approximately 1655 handover events per annum in our department. One hundred percent of physicians surveyed felt that documentation of handover was beneficial, and staff satisfaction with handover improved after initiation of the pilot (81 vs 24%, p = 0.000914). While 64% of staff were concerned that typed electronic handover would increase their workload, only 6% of the post pilot survey group felt that it did increase workload significantly.
Conclusion
Electronic clinical handover is feasible and practical within the Irish healthcare system. In addition, it was found in our study to be attractive and effective to physicians without increasing their workload.
Similar content being viewed by others
References
British Medical Association Junior Doctors Committee (2004) Safe handover: safe patients, guidance on clinical handover for clinicians and managers. BMA, London
The Royal College of Physicians; Acute care toolkit 1: Handover London: RCP, 2011
Schimmack S, Hinz U, Wagner A et al (2014) Maximizing time from the constraining European working time directive (EWTD): the Heidelberg new working time model. Heal Econ Rev 4:14. https://doi.org/10.1186/s13561-014-0014-6
The World Health Organisation; “Communication during patient hand-overs” Patient Safety Solutions; 2007. Vol 1, solution 3
The Joint Commisions Annual Report on Health and Safety, 2007
Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH (1994) Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med 121(11):866–872
Gottlieb DJ, Parenti CM, Peterson CA, Lofgren RP (1991) Effect of a change in house staff work schedule on resource utilization and patient care. Arch Intern Med 151(10):2065–2070
Lofgren RP, Gottlieb D, Williams RA, Rich EC (1990) Post-call transfer of resident responsibility: its effect on patient care. J Gen Intern Med 5(6):501–505
Laine C, Goldman L, Soukup JR, Hayes JG (1993) The impact of a regulation restricting medical house staff working hours on the quality of patient care. JAMA 269(3):374–378
Communication (Clinical Handover) in Acute and Children’s Hospital Services National Clinical Guideline No. 11
Murphy JN et al (2011) Handover rounds in Irish hospitals. Ir J Med Sci
Ryan S, O’Riordan JM, Tierney S, Conlon KC, Ridgway PF. Impact of a new electronic handover system in surgery.Int J Surg 2011;9(3):217–220. https://doi.org/10.1016/j.ijsu.2010.11.012. Epub 2010 Dec 1
Australian Commission on Safety and Quality in Health Care 2013
Starmer AJ, Spector ND, Srivastava R, West DC (2014) Changes in medical errors after implementation of a handoff program. N Engl J Med 371:1803–1812. https://doi.org/10.1056/NEJMsa1405556
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical statement
All authors state the following:
This manuscript has not been submitted elsewhere for consideration.
This manuscript has not been published previously.
No data has been fabricated or manipulated.
No data, text or theories have been plagiarised.
Consent to submit has been received explicitly from all authors.
All authors whose names appear on the manuscript have contributed to it sufficiently to share collective responsibility and accountability for the results.
Rights and permissions
About this article
Cite this article
Coughlan, J.J., Mross, T., Gul, F. et al. Implementing an electronic clinical handover system in a university teaching hospital. Ir J Med Sci 187, 309–312 (2018). https://doi.org/10.1007/s11845-017-1699-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-017-1699-4