Abstract
Background
Increasing demand exists for blended approaches to the development of professionalism. Trainees of the Royal College of Physicians of Ireland participated in an online patient safety programme.
Aims
Study aims were: (1) to determine whether the programme improved junior doctors’ knowledge, attitudes and skills relating to error reporting, open communication and care for the second victim and (2) to establish whether the methodology facilitated participants’ learning.
Methods
208 junior doctors who completed the programme completed a pre-online questionnaire. Measures were “patient safety knowledge and attitudes”, “medical safety climate” and “experience of learning”. Sixty-two completed the post-questionnaire, representing a 30 % matched response rate.
Results
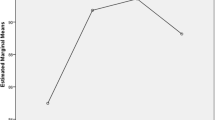
Participating in the programme resulted in immediate (p < 0.01) improvement in skills such as knowing when and how to complete incident forms and disclosing errors to patients, in self-rated knowledge (p < 0.01) and attitudes towards error reporting (p < 0.01). Sixty-three per cent disagreed that doctors routinely report medical errors and 42 % disagreed that doctors routinely share information about medical errors and what caused them. Participants rated interactive features as the most positive elements of the programme.
Conclusions
An online training programme on medical error improved self-rated knowledge, attitudes and skills in junior doctors and was deemed an effective learning tool. Perceptions of work issues such as a poor culture of error reporting among doctors may prevent improved attitudes being realised in practice. Online patient safety education has a role in practice-based initiatives aimed at developing professionalism and improving safety.

Similar content being viewed by others
References
Medical Council (2010) Eight Domains of Good Professional Practice as devised by the Medical Council. Available from: http://www.medicalcouncil.ie/Education-and-Training/Good-Professional-Practice/Eight-Domains-of-Good-Professional-Practice-as-devised-by-Medical-Council.pdf
Lukela MP, Parekh VI, Gosbee JW et al (2011) Competence in patient safety: a multi-faceted experiential educational intervention for resident physicians. J Grad Med Educ 3(3):360–366
Jansma JD, Wagner C, ten Kate RW et al (2011) Effects on incident reporting after educating residents in patient safety: a controlled study. BMC Health Serv Res 11:1–9
Kerfoot BP, Conlin PR, Travison T et al (2007) Patient safety knowledge and its determinants in medical trainees. J Gen Intern Med 22(8):150–1154
Cook DA, Beckman TJ, Thomas KG et al (2008) Adapting web-based instruction to residents’ knowledge improves learning efficiency: a randomized controlled trial. J Gen Intern Med 23(7):985–990
Merrill MD (2002) First principles of instruction. Educ Technol Res Dev 50(3):43–59
Ginsburg LR, Trequnno D, Norton PG (2013) Self-reported patient safety competence among new graduates in medicine, nursing and pharmacy. BMJ Qual Saf 22(2):147–154
Patrow CA, Kaprovich K, Riesenberg LA et al (2009) Residents’ engagement in quality improvement: a systematic review of the literature. Acad Med 84(12):1757–1764
Jansma JD, Wagner C, Bijnen AB (2010) Residents’ intentions and actions after patient safety education. BMC Health Serv Res 10:350–360
Swanick T (2012) Junior doctors: the best kept secret in the NHS. Postgrad Med J 88(1033):117–118
Shaw TJ, Pernar LI, Peyre SE et al (2012) Impact of online education on intern behaviour around joint commission national patient safety goals: a randomised trial. BMJ Qual Saf 21(10):819–825
World Alliance for Patient Safety (2008) WHO patient safety curriculum guide for medical schools. World Health Organisation, Switzerland
Case S, Swanson D (1996) Constructing written test questions for the basic and clinical sciences. National Board of Examiners, Philadelphia
Madigosky WS, Headrick LA, Nelson K et al (2006) Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med 81(1):94–100
Durani P, Dias J, Singh HP et al (2013) Junior doctors and patient safety: evaluating, knowledge, attitudes and perception of safety climate. BMJ Qual Saf 22(1):65–71
Robson J, de Wet C, McKay J et al (2011) Do we know what foundation year doctors think about patient safety incident reporting? Development of a web based tool to assess attitude and knowledge. Postgrad Med J 87(1033):750–756
White SM, Deacy N, Sudan S (2009) Trainee anaesthetists’ attitudes to error, safety and the law. Eur J Anaesthesiol 26(6):463–468
Flin R, Yule S, McKenzie L et al (2006) Attitudes to teamwork and safety in the operating theatre. Surgeon 4(3):145–151
Kaldjan LC, Jones EW, Wu BJ et al (2008) Reporting medical errors to improve patient safety: a survey of physicians in teaching hospitals. Arch Intern Med 168(1):40–46
Voss JD, May NB, Schorling JB et al (2008) Changing conversations: teaching safety and quality in residency training. Acad Med 83(11):1080–1087
Parker D, Lawton R (2003) Psychological contribution to the understanding of adverse events in healthcare. Qual Saf Health Care 12(6):453–457
West CP, Tan AD, Habermann TM et al (2009) Association of resident fatigue and distress with perceived medical errors. JAMA 302(12):1294–1300
Jagsi R, Kitch BT, Weinstein DF et al (2005) Residents report on adverse events and their causes. Arch Intern Med 165(22):2607–2613
Newman MC (1996) The emotional impact of mistakes on family physicians. Arch Fam Med 5(2):71–75
Wu AW, Folkman S, McPhee S et al (1991) Do house officers learn from their mistakes? JAMA 265(16):2089–2094
Mizrahi T (1984) Managing medical mistakes: ideology, insularity and accountability among internists-in-training. Soc Sci Med 19(2):135–146
Jericho BG, Tassone RF, Centomani NM et al (2010) An assessment of an educational intervention on resident physician attitudes, knowledge, and skills related to adverse event reporting. J Grad Med Educ 2(2):188–194
Mann S, Robertson IT (2006) What should training evaluations evaluate? J Eur Ind Train 20(9):14–20
Acknowledgments
The authors wish to thank Megan Burgdorf, RCPI, who contributed to the design of elements of the questionnaire and data collection and all those who completed questionnaires.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McCarthy, S.E., O’Boyle, C.A., O’Shaughnessy, A. et al. Online patient safety education programme for junior doctors: is it worthwhile?. Ir J Med Sci 185, 51–58 (2016). https://doi.org/10.1007/s11845-014-1218-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-014-1218-9