Abstract
Background
Cancer registries play a major role in cancer control, including quantifying the burden of cancer in the population, informing health service planning, and evaluating service provision. Registries must achieve a high level of completeness of case ascertainment.
Aim
Completeness of case ascertainment for the National Cancer Registry (NCR) in Ireland was estimated.
Methods
For all invasive cancers, and the four most common sites, we used two quantitative methods which use information from death certificates to obtain estimates of completeness of registration—the Lincoln–Petersen (LP) estimator (which provides a lower bound estimate) and the flow method (which estimates completeness at a fixed time-point, in this case 5 years). Data were extracted at the end of 2010. Independent case ascertainment was used to assess completeness of breast cancer registration in the 50–64 age group and of rectal cancer in surgical patients diagnosed in 2007.
Results
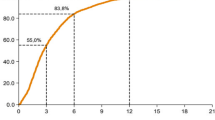
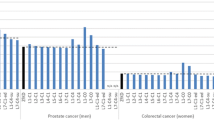
Completeness of case ascertainment was >99 % for the breast screening age-group and for surgical rectal cancer cases. A lower bound on completeness of case ascertainment for all invasive cancers excluding non-melanoma skin cancers is 94.3 % using the LP estimator. The estimate from the flow method is 97 % after 5 years, [95 % confidence interval (96.2 %, 97.7 %)]. Five-year levels of completeness for the four commonest cancers using the flow method were: colorectal, 97.4 %; lung, 98.7 %; prostate, 95.8 % and breast, 98.0 %.
Conclusion
The estimated levels of completeness for the NCR are satisfactory. Further work is required to compare the methods used.
Similar content being viewed by others
References
Brewster DH, Coebergh JW, Storm HH (2005) Population-based cancer registries: the invisible key to cancer control. Lancet Oncol 6(4):193–195
Brenner H, Hakulinen T (2005) Population-based monitoring of cancer patient survival in situations with imperfect completeness of cancer registration. Br J Cancer 92(3):576–579
Bray F, Parkin DM (2009) Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer 45(5):747–755
Parkin DM, Bray F (2009) Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer 45(5):756–764
Schmidtmann I, Blettner M (2009) How do cancer registries in Europe estimate completeness of registration? Methods Inf Med 48(3):267–271
Tyczynski JE, Demaret E, Parkin DM (2003) Standards and guidelines for cancer registration in Europe. IARC Technical Publication, vol 40. International Agency for Research on Cancer, Lyon
Bullard J et al (2000) Completeness of cancer registration: a new method for routine use. Br J Cancer 82(5):1111–1116
Comber H et al (2012) Quality of rectal cancer surgery and its relationship to surgeon and hospital caseload: a population-based study. Colorectal Dis 14(10):e692–e700
Hackl M, Waldhoer T (2012) Estimation of completeness of case ascertainment of Austrian cancer incidence data using the flow method. Eur J Public Health
Brewster DH et al (1997) Completeness of case ascertainment in a Scottish regional cancer registry for the year 1992. Public Health 111(5):339–343
Moller H et al (2011) Completeness of case ascertainment and survival time error in English cancer registries: impact on 1-year survival estimates. Br J Cancer 105(1):170–176
Larsen IK et al (2009) Data quality at the Cancer Registry of Norway: an overview of comparability, completeness, validity and timeliness. Eur J Cancer 45(7):1218–1231
Sigurdardottir LG et al (2012) Data quality at the Icelandic Cancer Registry: comparability, validity, timeliness and completeness. Acta Oncol 51(7):880–889
Schmidtmann I (2008) Estimating completeness in cancer registries—comparing capture–recapture methods in a simulation study. Biom J 50(6):1077–1092
Silcocks PB, Robinson D (2007) Simulation modelling to validate the flow method for estimating completeness of case ascertainment by cancer registries. J Public Health (Oxf) 29(4):455–462
Ferlay J et al (2013) Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 49(6):1374–1403
Sant M et al (2009) EUROCARE-4. Survival of cancer patients diagnosed in 1995–1999. Results and commentary. Eur J Cancer 45(6):931–991
Acknowledgments
We thank the Tumour Registration Officers and the Data Team of the National Cancer Registry who collect and process the data on which this paper was based.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Brien, K., Comber, H. & Sharp, L. Completeness of case ascertainment at the Irish National Cancer Registry. Ir J Med Sci 183, 219–224 (2014). https://doi.org/10.1007/s11845-013-0993-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-013-0993-z