Abstract
Nanoscience in healthcare offers significant advancement in the areas of diagnostic and therapeutic for imaging, biosensing, targeted drug delivery systems, etc. To extend the applications in biomedical engineering, artificial intelligence (AI) technology holds the power to analyze and interpret biological data, accelerate drug discovery and identify selective small molecules or unique compounds with predictive behavior. Implementation of such database systems for rapid data analysis, treatment strategies, novel hypotheses development, and determination of disease progression remarkably improves the treatment outcomes with the potential to accelerate the high-throughput development and systematic design of highly effective smart materials and nanoformulations with pre-defined functionality. Specifically, optimizing physicochemical parameters, compatibility, and drug-dose parameters with higher prediction efficiency (above 90%) is the area where AI holds the potential to actionably cognize the full nanotechnology potential. This review article discusses the research findings to accelerate the clinical translation of nanoscience, bestow the potential development of high throughput experimentation-based, AI-assisted design, and data-driven production of nanosynthesized systems.
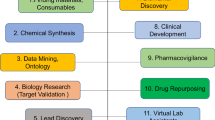
Graphical Abstract






Similar content being viewed by others
Abbreviations
- AI:
-
Artificial intelligence
- ML:
-
Machine learning
- DL:
-
Deep learning
- NN:
-
Neural network
- ANN:
-
Artificial neural network
- DNN:
-
Deep neural network
- CNN:
-
Convolutional neural network
- SPM:
-
Scanning probe microscopy
- PCA:
-
Principal component analysis
- PCL:
-
Poly(L-lactide)
- PLGA:
-
Poly(lactic-co-glycolic acid)
- EC:
-
Ethyl cellulose
- PLA:
-
Polylactic acid
- PEG:
-
Polyethylene glycol
- PVA:
-
Polyvinyl alcohol
- DLC:
-
Drug loading content
- DLE:
-
Drug loading efficiency
- DG:
-
Docking binding energy
- RMSE:
-
Root mean square error
- MAE:
-
Mean absolute error
- HLB:
-
Hydrophilic lipophilic balance
- DOX:
-
Doxorubicin
- MLP:
-
Multi-layer perceptron
- MON-MLP:
-
Monotome multi-layer perceptron
- QSPR:
-
Quantitative structure property relationships
- QSAR:
-
Quantitative structure activity relationship
- SVR:
-
Support vector regression
- HCA:
-
Hierarchical clustering algorithm
- LDA:
-
Linear discriminant analysis
- kNN:
-
K-nearest neighbors
- HUVEC:
-
Human umbilical vein endothelial cells
- GANDA:
-
Generative adversarial network for distribution analysis
- QD:
-
Quantum-dot
- ROI:
-
Region of interest
- MLR:
-
Multiple linear regression
- SERS:
-
Surface-enhanced raman spectroscopy
- HCG:
-
Human chronic gonadotropin
References
Ramesh AN, Kambhampati C, Monson J, Drew PJ (2004) Artificial intelligence in medicine. Ann R Coll Surg Engl. https://doi.org/10.1308/147870804290
Miles JC, Walker AJ (2006) The potential application of artificial intelligence in transport. IEE Proc: Intell Trans Syst 153:183–198. https://doi.org/10.1049/IP-ITS:20060014
Yang Y, Siau K (2018) A qualitative research on marketing and sales in the artificial intelligence age. MWAIS 2018 Proceedings
Wirtz BW, Weyerer JC, Geyer C (2018) Artificial intelligence and the public sector—applications and challenges. Int J Public Adm 42:596–615. https://doi.org/10.1080/01900692.2018.1498103
Rajaraman V (2014) JohnMcCarthy—father of artificial intelligence. Resonance 19:198–207. https://doi.org/10.1007/S12045-014-0027-9
Hamet P, Tremblay J (2017) Artificial intelligence in medicine. Metabolism 69:S36–S40. https://doi.org/10.1016/j.metabol.2017.01.011
Ekins S (2006) Computer methods for predicting drug metabolism. Comput Appl Pharm Res Dev. https://doi.org/10.1002/0470037237
Brady M (1985) Artificial intelligence and robotics. Artif Intell 26:79–121. https://doi.org/10.1016/0004-3702(85)90013-X
Murase H (2000) Artificial intelligence in agriculture. Comput Electron Agric 29:1–2. https://doi.org/10.1016/S0168-1699(00)00132-0
Cook DJ (2012) How smart is your home? Science 335:1579–1581. https://doi.org/10.1126/SCIENCE.1217640
Jiang F, Jiang Y, Zhi H et al (2017) Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol 2:230–243. https://doi.org/10.1136/SVN-2017-000101
Duch W, Swaminathan K, Meller J (2007) Artificial intelligence approaches for rational drug design and discovery. Curr Pharm Des 13:1497–1508. https://doi.org/10.2174/138161207780765954
Ardizzone E, Bonadonna F, Gaglio S et al (2009) Artificial intelligence techniques for cancer treatment planning. Med Inform 13:199–210. https://doi.org/10.3109/14639238809010100
Szolovits P, Patil RS, Schwartz WB (1988) Artificial intelligence in medical diagnosis. Ann Int Med 108(1):80. https://doi.org/10.7326/0003-4819-108-1-80
Hengstler M, Enkel E, Duelli S (2016) Applied artificial intelligence and trust—the case of autonomous vehicles and medical assistance devices. Technol Forecast Soc Change 105:105–120. https://doi.org/10.1016/J.TECHFORE.2015.12.014
Menezes G, Menez P, Meneze C (2011) Nanoscience in diagnostics: a short review. Internet J Med Update EJournal 6:16–23. https://doi.org/10.4314/ijmu.v6i1.63971
Hobson DW (2016) The commercialization of medical nanotechnology for medical applications. Intracell Delivery. https://doi.org/10.1007/978-3-319-43525-1_17
Laouini S, Laouini SE, Bouafia A, Tedjani ML (2021) Catalytic activity for dye degradation and characterization of silver/silver oxide nanoparticles green synthesized by aqueous leaves extract of phoenix Dactylifera L. https://doi.org/10.21203/RS.3.RS-139856/V1
Agarwal H, Venkat Kumar S, Rajeshkumar S (2017) A review on green synthesis of zinc oxide nanoparticles – an eco-friendly approach. Resource-Efficient Technol 3:406–413. https://doi.org/10.1016/J.REFFIT.2017.03.002
Bogutska КІ, Sklyarov YP, Prylutskyy Y (2013) Zinc and zinc nanoparticles: biological role and application in biomedicine. Ukr Bioorg Acta 1:9–16
Baker JR, Ward BB, Thomas T (2009) Nanotechnology in clinical and translational research. Clin Transl Sci: Princ Hum Res. https://doi.org/10.1016/B978-0-12-373639-0.00008-X
Shiku H, Wang L, Ikuta Y et al (2000) Development of a cancer vaccine: peptides, proteins, and DNA. Cancer Chemother Pharmacol 46:S77–S82. https://doi.org/10.1007/S002800000179
Saul JM, Annapragada A, Bellamkonda R (2006) A dual-ligand approach for enhancing targeting selectivity of therapeutic nanocarriers. J Controlled Release 114:277–287. https://doi.org/10.1016/J.JCONREL.2006.05.028
Shende P, Devlekar NP (2020) A review on the role of artificial intelligence in stem cell therapy: an initiative for modern medicines. Curr Pharm Biotechnol 22:1156–1163. https://doi.org/10.2174/1389201021666201007122524
Pathan N, Govardhane S, Shende P (2021) Stem cell progression for transplantation. Artif Intell Med. https://doi.org/10.1007/978-3-030-58080-3_336-1
Prajnamitra RP, Chen HC, Lin CJ et al (2019) Nanotechnology approaches in tackling cardiovascular diseases. Molecules 24:2017. https://doi.org/10.3390/MOLECULES24102017
Hastie T, Tibshirani R, Friedman J (2009) Overview of supervised learning. Elem Stat Learn Data Mining Inference Predict. https://doi.org/10.1007/978-0-387-84858-7_2
Wł Duch, Setiono R, Zurada JM (2004) Computational intelligence methods for rule-based data understanding. Proc IEEE 92:771–805. https://doi.org/10.1109/JPROC.2004.826605
Svetnik V, Liaw A, Tong C et al (2003) Random forest: a classification and regression tool for compound classification and QSAR modeling. J Chem Inf Comput Sci 43:1947–1958. https://doi.org/10.1021/CI034160G
Burden FR, Polley MJ, Winkler DA (2009) Toward novel universal descriptors: charge fingerprints. J Chem Inf Model 49:710–715. https://doi.org/10.1021/CI800290H
Le TC, Winkler DA (2016) Discovery and optimization of materials using evolutionary approaches. Chem Rev 116:6107–6132. https://doi.org/10.1021/ACS.CHEMREV.5B00691
Rashidi HH, Tran NK, Betts EV et al (2019) Artificial intelligence and machine learning in pathology: the present landscape of supervised methods. Acad Pathol 6:2374289519873088. https://doi.org/10.1177/2374289519873088
Hochreiter S (2011) The vanishing gradient Problem during Learning recurrent neural nets and Problem Solutions. Int J Uncertain Fuzzin Knowledge-Based Syst 6:107–116. https://doi.org/10.1142/S0218488598000094
Sathya Professor R, Nivas College J, Abraham Professor A (2013) Comparison of supervised and unsupervised learning algorithms for pattern classification. Int J Adv Res Artif Intell. https://doi.org/10.14569/IJARAI.2013.020206
Johnson KW, Torres Soto J, Glicksberg BS et al (2018) Artificial intelligence in cardiology. J Am Coll Cardiol 71:2668–2679. https://doi.org/10.1016/J.JACC.2018.03.521
Ghahramani, Z. (2003). Unsupervised learning. Summer school on machine learning. (72-112). https://doi.org/10.1007/978-3-540-28650-9_5
Jung E, Kim J, Choi SH et al (2010) Artificial neural network study on organ-targeting peptides. J Comput Aided Mol Des 24:49–56. https://doi.org/10.1007/S10822-009-9313-0
Mater AC, Coote ML (2019) Deep learning in chemistry. J Chem Inf Model. https://doi.org/10.1021/ACS.JCIM.9B00266
Hinton GE, Osindero SA (2006) A fast learning algorithm for deep belief nets. Neural Comput 18(7):1527–1554
Schmidhuber J (2014) Deep learning in neural networks: an overview. Neural Netw 61:85–117. https://doi.org/10.1016/j.neunet.2014.09.003
Gawehn E, Hiss JA, Schneider G (2016) Deep learning in drug discovery. Mol Inf 35:3–14. https://doi.org/10.1002/MINF.201501008
Krizhevsky A, Sutskever I, Hinton GE (2012) ImageNet classification with deep convolutional neural networks. Adv Neural Inf Process Syst 25:1
Sacha GM, Varona P (2013) Artificial intelligence in nanotechnology. Nanotechnology 24:452002. https://doi.org/10.1088/0957-4484/24/45/452002
Adir O, Poley M, Chen G et al (2020) Integrating artificial intelligence and nanotechnology for precision cancer medicine. Adv Mater 32:1901989. https://doi.org/10.1002/ADMA.201901989
Dana D, Gadhiya S, Surin LGS et al (2018) Deep learning in drug discovery and medicine, scratching the surface. Molecules 23:2384. https://doi.org/10.3390/MOLECULES23092384
Harashima H, Sakata K, Funato K, Kiwada H (1994) Enhanced hepatic uptake of liposomes through complement activation depending on the size of liposomes. Pharm Res: Of J Am Assoc Pharm Sci 11:402–406. https://doi.org/10.1023/A:1018965121222/METRICS
Ren J, Hong H, Song J, Ren T (2005) Particle size and distribution of biodegradable poly-D,L-lactide-co-poly(ethylene glycol) block polymer nanoparticles prepared by nanoprecipitation. J Appl Polym Sci 98:1884–1890. https://doi.org/10.1002/APP.22070
Kunjachan S, Detappe A, Kumar R et al (2015) Nanoparticle mediated tumor vascular disruption: a novel strategy in radiation therapy. Nano Lett 15:7488–7496. https://doi.org/10.1021/acs.nanolett.5b03073
Youshia J, Ali ME, Lamprecht A (2017) Artificial neural network based particle size prediction of polymeric nanoparticles. Eur J Pharm Biopharm 119:333–342. https://doi.org/10.1016/J.EJPB.2017.06.030
Li Y, Abbaspour MR, Grootendorst P et al (2015) Optimization of controlled release nanoparticle formulation of verapamil hydrochloride using artificial neural networks with genetic algorithm and response surface methodology. Eur J Pharm Biopharm 94:170–179. https://doi.org/10.1016/J.EJPB.2015.04.028
Shalaby KS, Soliman ME, Casettari L et al (2014) Determination of factors controlling the particle size and entrapment efficiency of noscapine in PEG/PLA nanoparticles using artificial neural networks. Int J Nanomedicine 9:4953–4964. https://doi.org/10.2147/IJN.S68737
Wu J, Zhu Y-J, Cao S-W et al (2010) Hierachically nanostructured mesoporous spheres of calcium silicate hydrate: surfactant-free sonochemical synthesis and drug-delivery system with ultrahigh drug-loading capacity. AdM 22:749–753. https://doi.org/10.1002/ADMA.200903020
Ribeiro CAS, de Castro CE, Albuquerque LJC et al (2017) Biodegradable nanoparticles as nanomedicines: are drug-loading content and release mechanism dictated by particle density? Colloid Polym Sci 295:1271–1280. https://doi.org/10.1007/S00396-016-4007-3
Trucillo P, Campardelli R, Reverchon E (2017) Supercritical CO2 assisted liposomes formation: optimization of the lipidic layer for an efficient hydrophilic drug loading. J CO2 Utilization 18:181–188. https://doi.org/10.1016/J.JCOU.2017.02.001
Metwally AA, Hathout RM (2015) Computer-assisted drug formulation design: novel approach in drug delivery. Mol Pharm 12:2800–2810. https://doi.org/10.1021/MP500740D
Esmaeilzadeh-Gharehdaghi E, Faramarzi MA, Amini MA et al (2014) Processing/formulation parameters determining dispersity of chitosan particles: an ANNs study. J Microencapsul 31:77–85. https://doi.org/10.3109/02652048.2013.805842
Makadia HK, Siegel SJ (2011) Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers 3:1377–1397. https://doi.org/10.3390/POLYM3031377
Husseini GA, Mjalli FS, Pitt WG, Abdel-Jabbar NM (2009) Using artificial neural networks and model predictive control to optimize acoustically assisted doxorubicin release from polymeric micelles. Tech Cancer Res Treat 8:479–488. https://doi.org/10.1177/153303460900800609
Szlek J, Pacławski A, Llau R et al (2013) Heuristic modeling of macromolecule release from PLGA microspheres. Int J Nanomed 8:4601–4611. https://doi.org/10.2147/IJN.S53364
Yadav S, Sharma AK, Kumar P (2020) Nanoscale self-assembly for therapeutic delivery. Front Bioeng Biotechnol 8:127. https://doi.org/10.3389/FBIOE.2020.00127
Li F, Han J, Cao T et al (2019) Design of self-assembly dipeptide hydrogels and machine learning via their chemical features. Proc Natl Acad Sci USA 166:11259–11264. https://doi.org/10.1073/PNAS.1903376116
Tu KH, Huang H, Lee S et al (2020) Machine learning predictions of block copolymer self-assembly. Adv Mater 32:2005713. https://doi.org/10.1002/ADMA.202005713
Govardhane S, Gandhi S, Shende P (2022) Neural-ensemble-based detection: a modern way to diagnose lung cancer. Artif Intell Cancer Diagn Progn. https://doi.org/10.1088/978-0-7503-3595-9CH2
Boso DP, Lee SY, Ferrari M et al (2011) Optimizing particle size for targeting diseased microvasculature: from experiments to artificial neural networks. Int J Nanomedicine 6:1517–1526. https://doi.org/10.2147/IJN.S20283
Bozuyuk U, Dogan NO, Kizilel S (2018) Deep insight into pegylation of bioadhesive chitosan nanoparticles: sensitivity study for the key parameters through artificial neural network model. ACS Appl Mater Interfaces 10:33945–33955. https://doi.org/10.1021/ACSAMI.8B11178
Bhatt M, Shende P (2023) Advancement in machine learning: a strategic lookout from cancer identification to treatment. Arch Comput Methods Eng 30(4):2777–2792. https://doi.org/10.1007/S11831-023-09886-0
Alafeef M, Srivastava I, Pan D (2020) Machine learning for precision breast cancer diagnosis and prediction of the nanoparticle cellular internalization. ACS Sens 5:1689–1698. https://doi.org/10.1021/ACSSENSORS.0C00329
Winkler DA, Burden FR, Yan B et al (2014) Modelling and predicting the biological effects of nanomaterials. SAR QSAR Environ Res 25:161–172. https://doi.org/10.1080/1062936X.2013.874367
Burden FR, Winkler DA (2009) Optimal sparse descriptor selection for QSAR using bayesian methods. QSAR Comb Sci 28:645–653. https://doi.org/10.1002/QSAR.200810173
Burden FR, Winkler DA (1999) Robust QSAR models using bayesian regularized neural networks. J Med Chem 42:3183–3187. https://doi.org/10.1021/JM980697N
Tang Y, Zhang J, He D et al (2021) GANDA: a deep generative adversarial network conditionally generates intratumoral nanoparticles distribution pixels-to-pixels. J Controlled Release 336:336–343. https://doi.org/10.1016/J.JCONREL.2021.06.039
Harrison PJ, Wieslander H, Sabirsh A et al (2021) Deep-learning models for lipid nanoparticle-based drug delivery. Nanomedicine 16:1097–1110. https://doi.org/10.2217/NNM-2020-0461
Wiedswang G, Næss AB, Naume B, Kaåresen R (2001) Micrometastasis to axillary lymph nodes and bone marrow in breast cancer patients. Breast 10:237–242. https://doi.org/10.1054/BRST.2000.0245
van den Brekell MWM, Stele H v., van der Valk P et al (1992) Micrometastases from squamous cell carcinoma in neck dissection specimens. Eur Arch Otorhinolaryngol 249:349–353. https://doi.org/10.1007/BF00179388
Kingston BR, Syed AM, Ngai J et al (2019) Assessing micrometastases as a target for nanoparticles using 3D microscopy and machine learning. Proc Natl Acad Sci USA 116:14937–14946. https://doi.org/10.1073/PNAS.1907646116
Banerjee A, Maity S, Mastrangelo CH (2021) Nanostructures for biosensing, with a brief overview on cancer detection, IoT, and the role of machine learning in smart biosensors. Sensors 21:1253. https://doi.org/10.3390/S21041253
Schluep T, Hwang J, Hildebrandt IJ et al (2009) Pharmacokinetics and tumor dynamics of the nanoparticle IT-101 from PET imaging and tumor histological measurements. Proc Natl Acad Sci USA 106:11394–11399. https://doi.org/10.1073/PNAS.0905487106
Villa Nova M, Lin TP, Shanehsazzadeh S et al (2022) Nanomedicine ex machina: between model-informed development and artificial intelligence. Front Digit Health 4:17. https://doi.org/10.3389/FDGTH.2022.799341
Cui F, Yue Y, Zhang Y et al (2020) Advancing biosensors with machine learning. ACS Sens 5:3346–3364. https://doi.org/10.1021/ACSSENSORS.0C01424
Erzina M, Trelin A, Guselnikova O et al (2020) Precise cancer detection via the combination of functionalized SERS surfaces and convolutional neural network with independent inputs. Sens Actuators B Chem 308:127660. https://doi.org/10.1016/J.SNB.2020.127660
Guselnikova O, Hrobonova K, Postnikov P et al (2017) Lipophilic gold grating for SERS detection of biological objects. Proceedings 1:4. https://doi.org/10.3390/PROCEEDINGS1040415
Yan W, Wang K, Xu H et al (2019) Machine learning approach to enhance the performance of MNP-labeled lateral flow immunoassay. Nanomicro Lett 11:1–15. https://doi.org/10.1007/S40820-019-0239-3
Pandit S, Banerjee T, Srivastava I et al (2019) Machine learning-assisted array-based biomolecular sensing using surface-functionalized carbon dots. ACS Sens 4:2730–2737. https://doi.org/10.1021/ACSSENSORS.9B01227
Furxhi I, Murphy F, Mullins M et al (2020) Practices and trends of machine learning application in nanotoxicology. Nanomaterials 10:116. https://doi.org/10.3390/NANO10010116
Lamon L, Asturiol D, Richarz A et al (2018) Grouping of nanomaterials to read-across hazard endpoints: from data collection to assessment of the grouping hypothesis by application of chemoinformatic techniques. Part Fibre Toxicol 15:1–17. https://doi.org/10.1186/S12989-018-0273-1
Epa VC, Burden FR, Tassa C et al (2012) Modeling biological activities of nanoparticles. Nano Lett 12:5808–5812. https://doi.org/10.1021/NL303144K
Horev-Azaria L, Baldi G, Beno D et al (2013) Predictive toxicology of cobalt ferrite nanoparticles: comparative in-vitro study of different cellular models using methods of knowledge discovery from data. Part Fibre Toxicol 10:1–17. https://doi.org/10.1186/1743-8977-10-32
Liu R, Jiang W, Walkey CD, Chan WCW, Cohen Y (2015) Prediction of nanoparticles-cell association based on corona proteins and physicochemical properties. Nanoscale 7(21):9664-9675. https://doi.org/10.1039/C5NR01537E
Manickam P, Mariappan SA, Murugesan SM et al (2022) Artificial intelligence (AI) and internet of medical things (IoMT) assisted biomedical systems for intelligent healthcare. Biosensors 12:562. https://doi.org/10.3390/BIOS12080562
Desai D, Shende P (2021) Integration of internet of things with quantum dots: a state-of-the-art of medicine. Curr Pharm Des 27:2068–2075. https://doi.org/10.2174/1381612827666210222113740
Ahmed S, Srinivasu PN, Alhumam A, Alarfaj M (2022) AAL and internet of medical things for monitoring type-2 diabetic patients. Diagnostics 12:2739. https://doi.org/10.3390/DIAGNOSTICS12112739
Wagan SA, Koo J, Siddiqui IF et al (2022) Internet of medical things and trending converged technologies: a comprehensive review on real-time applications. J King Saud Univ Comput Inform Sci 34:9228–9251. https://doi.org/10.1016/J.JKSUCI.2022.09.005
Hemmati A, Rahmani AM (2022) Internet of medical things in the COVID-19 Era: a systematic literature review. Sustainability 14:12637. https://doi.org/10.3390/SU141912637
Fang Y, Zou Y, Xu J et al (2021) Ambulatory cardiovascular monitoring via a machine-learning-assisted textile triboelectric sensor. Adv Mater 33:2104178. https://doi.org/10.1002/ADMA.202104178
Nakhleh MK, Baram S, Jeries R et al (2016) Artificially intelligent nanoarray for the detection of preeclampsia under real-world clinical conditions. Adv Mater Technol 1:1600132. https://doi.org/10.1002/ADMT.201600132
Lee HJ, Yang JC, Choi J et al (2021) Hetero-dimensional 2D Ti3C2TxMXene and 1D graphene nanoribbon hybrids for machine learning-assisted pressure sensors. ACS Nano 15:10347–10356. https://doi.org/10.1021/ACSNANO.1C02567
Luo M, Feng Y, Wang T, Guan J (2018) Micro-/nanorobots at work in active drug delivery. Adv Funct Mater 28:1706100. https://doi.org/10.1002/ADFM.201706100
Tripathi R, Kumar A (2018) Application of nanorobotics for cancer treatment. Mater Today Proc 5:9114–9117. https://doi.org/10.1016/J.MATPR.2017.10.029
Virgolino Glécia et al (2016) Nanorobotics in drug delivery systems for treatment of cancer: a review. J Mater Sci Eng A. https://doi.org/10.17265/2161-6213/2016.5-6.005
Mir UB, Sharma S, Kar AK, Gupta MP (2020) Critical success factors for integrating artificial intelligence and robotics. Digit Policy Regul Gov 22:307–331. https://doi.org/10.1108/DPRG-03-2020-0032
Fletcher M, Biglarbegian M, Neethirajan S (2013) Intelligent system design for bionanorobots in drug delivery. Cancer Nanotechnol 4:117–125. https://doi.org/10.1007/S12645-013-0044-5
He W, Frueh J, Hu N et al (2016) Guidable thermophoretic janus micromotors containing gold nanocolorifiers for infrared laser assisted tissue welding. Adv Sci 3:1600206. https://doi.org/10.1002/ADVS.201600206
Yan X, Zhou Q, Vincent M et al (2017) Multifunctional biohybrid magnetite microrobots for imaging-guided therapy. Sci Robot. https://doi.org/10.1126/SCIROBOTICS.AAQ1155. 2:
Hoop M, Ribeiro AS, Rösch D et al (2018) Mobile magnetic nanocatalysts for bioorthogonal targeted cancer therapy. Adv Funct Mater 28:1705920. https://doi.org/10.1002/ADFM.201705920
Baylis JR, Yeon JH, Thomson MH et al (2015) Self-propelled particles that transport cargo through flowing blood and halt hemorrhage. Sci Adv. https://doi.org/10.1126/SCIADV.1500379
Li J, Angsantikul P, Liu W et al (2017) Micromotors spontaneously neutralize gastric acid for pH-Responsive payload release. Angew Chem Int Ed 56:2156–2161. https://doi.org/10.1002/ANIE.201611774
Karshalev E, De Esteban-Fernández B, Beltrán-Gastélum M et al (2018) Micromotor pills as a dynamic oral delivery platform. ACS Nano 12:8397–8405. https://doi.org/10.1021/ACSNANO.8B03760
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kasture, K., Shende, P. Amalgamation of Artificial Intelligence with Nanoscience for Biomedical Applications. Arch Computat Methods Eng 30, 4667–4685 (2023). https://doi.org/10.1007/s11831-023-09948-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11831-023-09948-3