Abstract
Purpose
In patients receiving palliative care (PC), sleep is often negatively influenced by pain, anxiety and medication. Because these patients are often too sick to be investigated in a sleep laboratory, it is difficult to obtain objective information concerning their sleep. This study investigates whether bispectral index (BIS) monitoring reflects wakefulness, sleep and the effect of medication and whether it is tolerable for patients.
Methods
In all, 10 patients from an inpatient PC unit participated in the study. They were monitored using a BIS system for one night, while each event was carefully documented by patient care attendants. In addition, participants completed a questionnaire on the evening prior to and on the morning following the recording about their subjective wellbeing and sleep.
Results
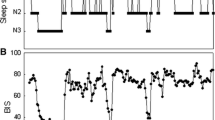
On a scale from 0 to 100, BIS measurements covered values ranging from a minimum of 29–40 to a maximum of 74–98. Individual differences between minimum and maximum ranged between 38 and 68. High BIS values are associated with wakefulness, low BIS values with sleep. The administration of sedative and analgesic medication was followed by a long-lasting decrease in BIS measurements. In 3 patients, the measurements were discontinued due to the patient being disturbed or irritation of the skin.
Conclusion
BIS monitoring was well tolerated by most but not all patients. It can be useful in complementing patients’ reports in questionable cases. This might be of special interest in outpatient settings where continuous objective professional observation is not available.
Zusammenfassung
Hintergrund
Erholsamer Schlaf ist wichtig für die Lebensqualität von Palliativpatienten, wird aber oftmals negativ durch Schmerzen, Angst und Medikamente beeinflusst. Da die Patienten für eine Untersuchung im Schlaflabor meistens zu krank sind, ist es schwierig, objektive Informationen über ihren Schlaf zu erhalten. Die Studie untersucht, ob das Bispectral-Index(BIS)-Monitoring den nächtlichen Verlauf von Schlaf und Wachheit sowie die Auswirkung verschiedener Medikamente widerspiegelt und ob die Messmethode für Palliativpatienten tolerabel ist.
Methoden
In der Zeit zwischen November 2010 und Februar 2011 nahmen 10 Patienten der Palliativstation am Universitätsklinikum Aachen an der Studie teil. Sie wurden während einer Nacht mit dem BIS-Monitorsystem untersucht, und jedes Ereignis während des Schlafs wurde von Sitzwachen dokumentiert. Zudem beantworteten die Studienteilnehmer am Abend vor und am Morgen nach der Messung Fragebögen über ihr subjektives Wohlbefinden und ihren Schlaf.
Ergebnisse
Auf einer Skala zwischen 0 und 100 lagen die gemessenen BIS-Werte minimal zwischen 29 und 40 und maximal zwischen 74 und 98. Der individuelle Unterschied zwischen Minimum und Maximum variierte zwischen 38 und 68. Hohe BIS-Werte konnten mit Wachheit in Verbindung gebracht werden, niedrige mit Schlaf. Die Gabe von sedierenden und analgetischen Medikamenten hatte einen lange andauernden Abfall der Werte zur Folge. Bei 3 Patienten musste die Messung wegen Störgefühlen oder Hautrötungen abgebrochen werden.
Schlussfolgerungen
Mit dem BIS-Monitoring konnte der Verlauf von Schlaf und Wachheit gut abgebildet werden. Die Messungen wurden von der Mehrheit, aber nicht von allen Patienten toleriert. Die Methode könnte auch im ambulanten Setting helfen, subjektive Angaben der Patienten zum Schlaf und Auswirkungen von Medikamenten weiter zu untersuchen.





Similar content being viewed by others
References
Avidan MS, Jacobsohn E, Glick D et al (2011) Prevention of intraoperative awareness in a high-risk surgical population. N Engl J Med 365(7):591–600
Barbato M (2001) Bispectral index monitoring in unconscious palliative care patients. J Palliat Care 17(2):102–108
Bestas A, Yasar MA, Bayar MK, Inalkac S (2004) The effects of two different anaesthesia techniques on bispectral index values and awareness during off-pump coronary artery bypass grafting. J Clin Monit Comput 18(5–6):347–351
Bourne RS, Minelli C, Mills GH, Kandler R (2007) Clinical review: sleep measurement in critical care patients: research and clinical implications. Crit Care 11(4):226
Buchanan FF, Myles PS, Cicuttini F (2011) Effect of patient sex on general anaesthesia and recovery. Br J Anaesth 106(6):832–839
Carozzi C, Rampil IJ (2011) Bispectral index for sleep screening: it is time to move on. Minerva Anestesiol 77(5):485–487
Dahaba AA, Xue JX, Xu GX et al (2011) Bilateral Bispectral Index (BIS)-Vista as a measure of physiologic sleep in sleep-deprived anesthesiologists. Minerva Anestesiol 77(4):388–393
Dijk DJ, Groeger JA, Stanley N, Deacon S (2010) Age-related reduction in daytime sleep propensity and nocturnal slow wave sleep. Sleep 33(2):211–223
Gambrell M (2005) Using the BIS monitor in palliative care: a case study. J Neurosci Nurs 37(3):140–143
Gan TJ, Glass PS, Windsor A et al (1997) Bispectral index monitoring allows faster emergence and improved recovery from propofol, alfentanil, and nitrous oxide anesthesia. BIS Utility Study Group. Anesthesiology 87(4):808–815
German Sleep Society (2007, Abend/Morgenprotokolle http://www.charite.de/dgsm/dgsm/downloads/fachinformationen/frageboegen/protokol.pdf. Accessed 29 Apr 2013
Gibbins J, McCoubrie R, Kendrick AH et al (2009) Sleep-wake disturbances in patients with advanced cancer and their family carers. J Pain Symptom Manage 38(6):860–870
Grond S, Zech D, Diefenbach C, Bischoff A (1994) Prevalence and pattern of symptoms in patients with cancer pain: a prospective evaluation of 1635 cancer patients referred to a pain clinic. J Pain Symptom Manage 9(6):372–382
Horiuchi T, Kawaguchi M, Kurita N et al (2007) The validity of bispectral index values from a dislocated sensor: a comparison with values from a sensor located in the commercially recommended position. Anesth Analg 104(4):857–859
Knudsen AK, Brunelli C, Klepstad P et al (2012) Which domains should be included in a cancer pain classification system? Analyses of longitudinal data. Pain 153(3):696–703
Leger D, Bayon V (2010) Societal costs of insomnia. Sleep Med Rev 14(6):379–389
Myles PS, Leslie K, McNeil J et al (2004) Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 363(9423):1757–1763
Mystakidou K, Parpa E, Tsilika E et al (2007) Depression, hopelessness, and sleep in cancer patients’ desire for death. Int J Psychiatry Med 37(2):201–211
Mystakidou K, Parpa E, Tsilika E et al (2007) The relationship of subjective sleep quality, pain, and quality of life in advanced cancer patients. Sleep 30(6):737–742
Nieuwenhuijs D, Coleman EL, Douglas NJ et al (2002) Bispectral index values and spectral edge frequency at different stages of physiologic sleep. Anesth Analg 94(1):125–129
Okifuji A, Hare BD (2011) Nightly analyses of subjective and objective (actigraphy) measures of sleep in fibromyalgia syndrome: what accounts for the discrepancy? Clin J Pain 27(4):289–296
Radbruch L, Nauck F, Ostgathe C et al (2003) What are the problems in palliative care? Results from a representative survey. Support Care Cancer 11(7):442–451
Rampil IJ (1998) A primer for EEG signal processing in anesthesia. Anesthesiology 89(4):980–1002
Savard J, Morin CM (2001) Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol 19(3):895–908
Sleigh JW, Andrzejowski J, Steyn-Ross A, Steyn-Ross M (1999) The bispectral index: a measure of depth of sleep? Anesth Analg 88(3):659–661
Stiel S, Matthes ME, Bertram L et al (2010) Validation of the new version of the minimal documentation system (MIDOS) for patients in palliative care: the German version of the Edmonton Symptom Assessment Scale (ESAS). Schmerz 24(6):596–604
Takahashi S, Sakai T, Matsuki A (1999) Relationship between bispectral index and sleep stages in man. Anesth Analg-Abstracts 88:57–58
Theobald DE (2004) Cancer pain, fatigue, distress, and insomnia in cancer patients. Clin Cornerstone 6(Suppl 1D):S15–S21
Tufano R, Palomba R, Lambiase G, Giurleo LG (2000) The utility of bispectral index monitoring in general anesthesia. Minerva Anestesiol 66(5):389–393
Vanable PA, Aikens JE, Tadimeti L et al (2000) Sleep latency and duration estimates among sleep disorder patients: variability as a function of sleep disorder diagnosis, sleep history, and psychological characteristics. Sleep 23(1):71–79
Wang MY, Hung HL, Tsai PS (2011) The sleep log and actigraphy: congruency of measurement results for heart failure patients. J Nurs Res 19(3):173–180
Acknowledgements
We gratefully thank Covidien (Neustadt an der Donau, Germany) for loaning a BIS VISTA™ to us for the time of the study. The company did not influence the results or the writing of the manuscript in any way.
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Linda Bertram and Stephanie Stiel contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Bertram, L., Stiel, S., Krumm, N. et al. Bispectral index monitoring of sleep in palliative care patients. Somnologie 17, 115–121 (2013). https://doi.org/10.1007/s11818-013-0612-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11818-013-0612-2