Abstract
Purpose
To perform a systematic review identifying how dietary factors are related to cognitive function in cancer survivors who are not currently undergoing primary treatment.
Methods
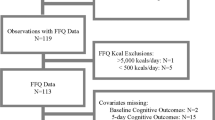
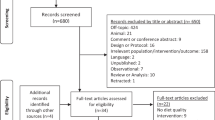
Using the PRISMA framework, a search was conducted for studies published before February 2019 across multiple databases, identifying 2304 unique articles. Twelve met final inclusion criteria and were evaluated through narrative synthesis. This review was registered with the International Prospective Register Of Systematic Reviews (CRD42018111941).
Results
Included studies were heterogeneous in methodology and in dietary and cognitive variables investigated making direct comparisons difficult. Evidence of a relationship between diet and cognition was mixed; the most consistent evidence was identified in relation to a positive relationship between fruit and vegetable intake and cognitive function (both self-reported and objectively tested) in five out of six studies, but was not concordant across all studies.
Conclusion
Preliminary evidence exists that a greater fruit and vegetable intake is associated with better cognitive functioning in cancer survivors, as has been reported in healthy populations; however, these data are correlational and include relatively small samples. Most evidence related to breast cancer survivors, with individual studies extending to colorectal and stomach cancer survivors. Experimental trials are needed to identify causal attribution of dietary factors on cognitive function in cancer survivors.
Implications for cancer survivors
At this time, there is not sufficient evidence to make dietary or nutritional recommendations specifically for improving cognitive function in cancer survivors. This should be considered in light of the general paucity of research on this subject, necessitating further investigations.

Similar content being viewed by others
References
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271–89. https://doi.org/10.3322/caac.21349.
International Agency for Research on Cancer. GLOBOCAN 2012: Estimated Cancer incidence, Mortality and Prevalence Worldwise in 2012; 2018. http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed 1 May 2019.
Janelsins MC, Kesler SR, Ahles TA, Morrow GR. Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry. 2014;26(1):102–13. https://doi.org/10.3109/09540261.2013.864260.
Lange M, Joly F. How to identify and manage cognitive dysfunction after breast cancer treatment. J Oncol Pract. 2017;13(12):784–90. https://doi.org/10.1200/JOP.2017.026286.
Beilharz JE, Maniam J, Morris MJ. Diet-induced cognitive deficits: the role of fat and sugar, potential mechanisms and nutritional interventions. Nutrients. 2015;7(8):6719–38. https://doi.org/10.3390/nu7085307.
Reichelt A, Stoeckel L, Reagan L, Winstanley C, Page K. Dietary influences on cognition. Physiol Behav. 2018;192:118–26. https://doi.org/10.1016/j.physbeh.2018.02.052.
Rodriguez RL, Albeck JG, Taha AY, Ori-McKenney KM, Recanzone GH, Stradleigh TW, et al. Impact of diet-derived signaling molecules on human cognition: exploring the food–brain axis npj. Sci Food. 2017;1(1):1–2. https://doi.org/10.1038/s41538-017-0002-4.
Zimmer P, Baumann FT, Oberste M, Wright P, Garthe A, Schenk A, et al. Effects of exercise interventions and physical activity behavior on cancer related cognitive impairments: a systematic review. Biomed Res Int. 2016;2016:1–13. https://doi.org/10.1155/2016/1820954.
Ahles TA, Root JC. Cognitive effects of cancer and cancer treatments. Annu Rev Clin Psychol. 2018;14:425–51. https://doi.org/10.1146/annurev-clinpsy-050817-084903.
Wefel JS, Kesler SR, Noll KR, Schagen SB. Clinical characteristics, pathophysiology, and management of noncentral nervous system cancer-related cognitive impairment in adults. CA Cancer J Clin. 2015;65(2):123–38.
Von Ah D, Habermann B, Carpenter JS, Schneider BL. Impact of perceived cognitive impairment in breast cancer survivors. Eur J Oncol Nurs. 2013;17(2):236–41. https://doi.org/10.1016/j.ejon.2012.06.002.
Myers J. Chemotherapy-related cognitive impairment: the breast cancer experience. Oncol Nurs Forum. 2012;39(1):E31–40. https://doi.org/10.1188/12.ONF.E31-E40.
Wieneke MH, Dienst ER. Neuropsychological assessment of cognitive functioning following chemotherapy for breast cancer. Psycho-Oncology. 1995;4(1):61–6. https://doi.org/10.1002/pon.2960040108.
Kucherer S, Ferguson RJ. Cognitive behavioral therapy for cancer-related cognitive dysfunction. Curr Opin Support Palliat Care. 2017;11(1):46–51. https://doi.org/10.1097/SPC.0000000000000247.
Valpey RE. Cancer-related cognitive impairment: considering risk factors, approaching assessment, and contemplating treatment. Am J Geriatr Psychiatry. 2017;25(12):1427–8. https://doi.org/10.1016/j.jagp.2017.09.015.
Boykoff N, Moieni M, Subramanian SK. Confronting chemobrain: an in-depth look at survivors’ reports of impact on work, social networks, and health care response. J Cancer Surviv. 2009;3(4):223–32.
Mayo S, Messner H, Rourke S, Howell D, Victor J, Kuruvilla J, et al. Relationship between neurocognitive functioning and medication management ability over the first 6 months following allogeneic stem cell transplantation. Bone Marrow Transplant. 2016;51(6):841–7. https://doi.org/10.1038/bmt.2016.2.
Wefel JS, Lenzi R, Theriault RL, Davis RN, Meyers CA. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma. Cancer. 2004;100(11):2292–9. https://doi.org/10.1002/cncr.20272.
Bray VJ, Dhillon HM, Vardy JL. (eds) Cancer-related cognitive impairment in adult cancer survivors: a review of the literature. Cancer Forum; 2017: The Cancer Council Australia.
Walker C, Drew BA, Antoon JW, Kalueff AV, Beckman BS. Neurocognitive effects of chemotherapy and endocrine therapies in the treatment of breast cancer: recent perspectives. Cancer Investig. 2012;30(2):135–48. https://doi.org/10.3109/07357907.2011.636116.
Orchard TS, Gaudier-Diaz MM, Weinhold KR, Courtney DVA. Clearing the fog: a review of the effects of dietary omega-3 fatty acids and added sugars on chemotherapy-induced cognitive deficits. Breast Cancer Res Treat. 2017;161(3):391–8. https://doi.org/10.1007/s10549-016-4073-8.
Grosso G, Bella F, Godos J, Sciacca S, Del Rio D, Ray S, et al. Possible role of diet in cancer: systematic review and multiple meta-analyses of dietary patterns, lifestyle factors, and cancer risk. Nutr Rev. 2017;75(6):405–19.
Lucchiari C, Masiero M, Pravettoni G. Methods for nutrition monitoring in cancer patients: a cognitive perspective. Ecancermedicalscience. 2012;6:259. https://doi.org/10.3332/ecancer.2012.259.
Schwedhelm C, Boeing H, Hoffmann G, Aleksandrova K, Schwingshackl L. Effect of diet on mortality and cancer recurrence among cancer survivors: a systematic review and meta-analysis of cohort studies. Nutr Rev. 2016;74(12):737–48. https://doi.org/10.1093/nutrit/nuw045.
Petersson SD, Philippou E. Mediterranean diet, cognitive function, and dementia: a systematic review of the evidence. Adv Nutr. 2016;7(5):889–904. https://doi.org/10.3945/an.116.012138.
Mustian K, Sprod L, Janelsins M, Peppone L, Mohile S. Exercise recommendations for cancer-related fatigue, cognitive impairment, sleep problems, depression, pain, anxiety, and physical dysfunction: a review. Oncol Hematol Rev. 2012;8(2):81–8.
Myers J, Erickson KI, Sereika SM, Bender CM. Exercise as an intervention to mitigate decreased cognitive function from cancer and cancer treatment: an integrative review. Cancer Nurs. 2018;41(4):327–43.
Beeken R, Williams K, Wardle J, Croker H. “What about diet?” a qualitative study of cancer survivors' views on diet and cancer and their sources of information. Eur J Cancer Care. 2016;25(5):774–83. https://doi.org/10.1111/ecc.12529.
Hodgson KD, Hutchinson AD, Wilson CJ, Nettelbeck T. A meta-analysis of the effects of chemotherapy on cognition in patients with cancer. Cancer Treat Rev. 2013;39(3):297–304.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
National Health Medical Research Council. How to review the evidence: systematic identification and review of the scientific literature. Canberra: NHMRC; 2000.
Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. 2016;6(12):e011458.
Joanna Briggs Institute. Critical Appraisal Tools: Checklist for Quasi-Experimental Studies. 2018. https://joannabriggs.org/sites/default/files/2019-05/JBI_Quasi-Experimental_Appraisal_Tool2017_0.pdf. Accessed 15 Apr 2019.
Huang Z, Shi Y, Bao P, Cai H, Hong Z, Ding D, et al. Associations of dietary intake and supplement use with post-therapy cognitive recovery in breast cancer survivors. Breast Cancer Res Treat. 2018;171(1):189–98. https://doi.org/10.1007/s10549-018-4805-z.
George SM, Alfano CM, Neuhouser ML, Smith AW, Baumgartner RN, Baumgartner KB, et al. Better postdiagnosis diet quality is associated with less cancer-related fatigue in breast cancer survivors. J Cancer Surviv. 2014;8(4):680–7.
Befort CA, Klemp JR, Austin HL, Perri MG, Schmitz KH, Sullivan DK, et al. Outcomes of a weight loss intervention among rural breast cancer survivors. Breast Cancer Res Treat. 2012;132(2):631–9. https://doi.org/10.1007/s10549-011-1922-3.
Gong XH, Wang JW, Li J, Chen XF, Sun L, Yuan ZP, et al. Physical exercise, vegetable and fruit intake and health-related quality of life in Chinese breast cancer survivors: a cross-sectional study. Qual Life Res. 2017;26(6):1541–50.
Grimmett C, Bridgewater J, Steptoe A, Wardle J. Lifestyle and quality of life in colorectal cancer survivors. Qual Life Res Int J Qual Life Asp Treat Care Rehab. 2011;20(8):1237–45.
Kanera IM, Bolman CA, Mesters I, Willems RA, Beaulen AA, Lechner L. Prevalence and correlates of healthy lifestyle behaviors among early cancer survivors. BMC Cancer. 2016;16:4.
Mohammadi S, Sulaiman S, Koon PB, Amani R, Hosseini SM. Impact of healthy eating practices and physical activity on quality of life among breast cancer survivors. Asian Pac J Cancer Prev. 2013;14(1):481–7.
Nomura SJ, Hwang Y-T, Gomez SL, Fung TT, Yeh S-L, Dash C, et al. Dietary intake of soy and cruciferous vegetables and treatment-related symptoms in Chinese-American and non-Hispanic White breast cancer survivors. Breast Cancer Res Treat. 2018;168(2):467–79.
Wang JW, Zhang CG, Deng QL, Chen WL, Wang X, Yu JM. The associations of comorbidities and consumption of fruit and vegetable with quality of life among stomach cancer survivors. Health Qual Life Outcomes. 2018;16. https://doi.org/10.1186/s12955-018-0886-y.
Zuniga KE, Mackenzie MJ, Roberts SA, Raine LB, Hillman CH, Kramer AF, et al. Relationship between fruit and vegetable intake and interference control in breast cancer survivors. Eur J Nutr. 2016;55(4):1555–62. https://doi.org/10.1007/s00394-015-0973-3.
Zuniga KE, Moran NE. Low serum carotenoids are associated with self-reported cognitive dysfunction and inflammatory markers in breast cancer survivors. Nutrients. 2018;10:8. https://doi.org/10.3390/nu10081111.
Kim NH, Song S, Jung SY, Lee E, Kim Z, Moon HG, et al. Dietary pattern and health-related quality of life among breast cancer survivors. BMC Womens Health. 2018;18:65. https://doi.org/10.1186/s12905-018-0555-7.
Fraser PD, Bramley PM. The biosynthesis and nutritional uses of carotenoids. Prog Lipid Res. 2004;43(3):228–65.
National Health and Medical Research Council. Serving Sizes. 2015. https://www.eatforhealth.gov.au/food-essentials/how-much-do-we-need-each-day/serve-sizes. Accessed 1 May 2019.
Marmot M, Atinmo T, Byers T, Chen J, Hirohata T, Jackson A et al. Food, nutrition, physical activity, and the prevention of cancer: a global perspective: World Cancer Research Fund/American Institute for Cancer Research; 2007.
Ahles TA, Hurria A. New challenges in psycho-oncology research IV: cognition and cancer: conceptual and methodological issues and future directions. Psycho-oncology. 2018;27(1):3–9.
McNaughton S, Hughes M, Marks G. Validation of a FFQ to estimate the intake of PUFA using plasma phospholipid fatty acids and weighed foods records. Br J Nutr. 2007;97(3):561–8.
Bhushan A, Fondell E, Ascherio A, Yuan C, Grodstein F, Willett W. Adherence to Mediterranean diet and subjective cognitive function in men. Eur J Epidemiol. 2018;33(2):223–34.
Fabbri AD, Crosby GA. A review of the impact of preparation and cooking on the nutritional quality of vegetables and legumes. Int J Gastron Food Sci. 2016;3:2–11.
Food Standards Australia New Zealand. Download Excel files (Australian Food Composition Database) - Nutrient File - Release 1. 2019. http://www.foodstandards.gov.au/science/monitoringnutrients/afcd/Pages/downloadableexcelfiles.aspx. Accessed 1 May 2019.
Dyall SC. Long-chain omega-3 fatty acids and the brain: a review of the independent and shared effects of EPA, DPA and DHA. Front Aging Neurosci. 2015;7:52. https://doi.org/10.3389/fnagi.2015.00052.
Wilcox S, Sharkey JR, Mathews AE, Laditka JN, Laditka SB, Logsdon RG, et al. Perceptions and beliefs about the role of physical activity and nutrition on brain health in older adults. The Gerontologist. 2009;49(S1):S61–71.
Mengelberg A, Leathem J, Podd J. Fish oil supplement use in New Zealand: a cross-sectional survey. Complement Ther Clin Pract. 2018;33:118–23.
Kent K, Charlton KE, Netzel M, Fanning K. Food-based anthocyanin intake and cognitive outcomes in human intervention trials: a systematic review. J Hum Nutr Diet. 2017;30(3):260–74.
Hammond BR Jr, Miller LS, Bello MO, Lindbergh CA, Mewborn C, Renzi-Hammond LM. Effects of lutein/zeaxanthin supplementation on the cognitive function of community dwelling older adults: a randomized, double-masked, placebo-controlled trial. Front Aging Neurosci. 2017;9(254):1–9.
Kang JH, Ascherio A, Grodstein F. Fruit and vegetable consumption and cognitive decline in aging women. Ann Neurol. 2005;57(5):713–20.
Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Econ. 1993;2(3):217–27.
Sharma P, Wisniewski A, Braga-Basaria M, Xu X, Yep M, Denmeade S, et al. Lack of an effect of high dose isoflavones in men with prostate cancer undergoing androgen deprivation therapy. J Urol. 2009;182(5):2265–73. https://doi.org/10.1016/j.juro.2009.07.030.
Acknowledgments
The authors would like to acknowledge the work of the research assistant Daria Gutteridge for her assistance with study screening. This research was made possible thanks to the Australian Government Research Training Program (RTP) fee offset scholarship funding DC.
Author information
Authors and Affiliations
Contributions
DC contributed to the study conception and design, overall study coordination, data collection/screening/ reduction/interpretation, sourcing funds, analysis of data, and drafting and writing the manuscript. AH and AC contributed to study conception and design, data screening/interpretation, overall study coordination, advice on analysis, and drafting the manuscript. AC additionally contributed to data collection. SD contributed to data collection/cleaning/analysis, and drafting the manuscript. SB contributed to study conception and design, overall study coordination, sourcing funds, advice on analysis, and drafting the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This review does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 48 kb)
Rights and permissions
About this article
Cite this article
Coro, D., Hutchinson, A., Dahlenburg, S. et al. The relationship between diet and cognitive function in adult cancer survivors: a systematic review. J Cancer Surviv 13, 773–791 (2019). https://doi.org/10.1007/s11764-019-00796-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-019-00796-4