Abstract
Purpose
Despite the life-threatening character of allogeneic hematopoietic stem cell transplantation (allogeneic HSCT), very few longitudinal research exists on posttraumatic stress disorder (PTSD) symptomatology in this patient group. We investigated prevalence, temporal course and predictors of PTSD symptomatology in this population.
Methods
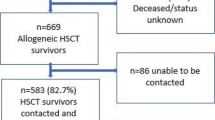
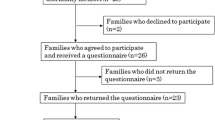
Patients were assessed before conditioning (T0), 100 days (T1), and 12 months after HSCT (T2). PTSD symptomatology was measured with the PTSD Checklist—Civilian Version. We conducted multilevel modeling and multiple regression analyses.
Results
Two hundred thirty-nine patients participated at baseline, 150 at T1, and 102 at T2. Up to 15 % met the criteria for PTSD at least once during the course of assessment. Fifty-two percent showed diagnostic relevant levels of intrusion, 30 % of avoidance, and 33 % of arousal at least once. Apart from arousal, which increased between T0 and T1 (γ = 0.56, p = 0.03), no other severity score significantly differed between time points. Being impaired by pain (γ = 2.89, p < 0.01), pain level (γ = 0.63, p = 0.02), and being female (γ = 3.81, p < 0.01) emerged as significant predictors of PTSD symptomatology when taking into account all time points. Acute plus chronic graft-versus-host-disease and longer hospital stay predicted PTSD symptomatology at T2 (γ = 3.39, p = 0.04; γ = 0.1, p = 0.03).
Conclusions
A considerable number of patients undergoing allogeneic HSCT met the criteria for PTSD. PTSD symptomatology is prominent at all assessment points. Burden of pain, being female, and medical complications are risk factors for elevated levels of PTSD symptomatology.
Implications for cancer survivors
Psychological support should be offered not only after treatment but also in the long-term and even before HSCT. Professionals should be aware of the psychological consequences accompanied by pain and complications.
Similar content being viewed by others
References
Hefner J, Kapp M, Drebinger K, et al. High prevalence of distress in patients after allogeneic hematopoietic SCT: fear of progression is associated with a younger age. Bone Marrow Transplant. 2014;49:581–4.
Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354:1813–26.
Kurosawa S, Yamaguchi T, Mori T, et al. Patient-reported quality of life after allogeneic hematopoietic cell transplantation or chemotherapy for acute leukemia. Bone Marrow Transplant. 2015;50:1241–9.
Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psychooncology. 2009;18:113–27.
Cooke L, Gemmill R, Kravits K, Grant M. Psychological issues of stem cell transplant. Semin Oncol Nurs. 2009;25:139–50.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. DSM-IV. 4th ed. Washington, DC: American Psychiatric Association; 1994.
Lee SJ, Loberiza FR, Antin JH, et al. Routine screening for psychosocial distress following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2005;35:77–83.
DuHamel KN, Ostrof J, Ashman T, et al. Construct validity of the posttraumatic stress disorder checklist in cancer survivors: analyses based on two samples. Psychol Assess. 2004;16:255–66.
Jacobsen PB, Sadler IJ, Booth-Jones M, Soety E, Weitzner MA, Fields KK. Predictors of posttraumatic stress disorder symptomatology following bone marrow transplantation for cancer. J Consult Clin Psychol. 2002;70:235–40.
Smith MY, Redd W, DuHamel K, Vickberg SJ, Ricketts P. Validation of the PTSD checklist—civilian version in survivors of bone marrow transplantation. J Trauma Stress. 1999;12:485–99.
Widows MR, Jacobsen PB, Fields KK. Relation of psychological vulnerability factors to posttraumatic stress disorder symptomatology in bone marrow transplant recipients. Psychosom Med. 2000;62:873–82.
Jacobsen PB, Widows MR, Hann DM, Andrykowski MA, Kronish LE, Fields KK. Posttraumatic stress disorder symptoms after bone marrow transplantation for breast cancer. Psychosom Med. 1998;60:366–71.
Wettergren L, Langius A, Bjorkholm M, Bjorvell H. Post-traumatic stress symptoms in patients undergoing autologous stem cell transplantation. Acta Oncol. 1999;38:475–80.
Voigt V, Neufeld F, Kaste J, et al. Clinically assessed posttraumatic stress in patients with breast cancer during the first year after diagnosis in the prospective, longitudinal, controlled COGNICARES study. Psychooncology. 2016.
Smith SK, Zimmerman S, Williams CS, et al. Post-traumatic stress symptoms in long-term non-Hodgkin’s lymphoma survivors: does time heal? J Clin Oncol. 2011;29:4526–33.
DuHamel KN, Smith MY, Vickberg SM, et al. Trauma symptoms in bone marrow transplant survivors: the role of nonmedical life events. J Trauma Stress. 2001;14:95–113.
Tan G, Fink B, Dao TK, et al. Associations among pain, PTSD, mTBI, and heart rate variability in veterans of Operation Enduring and Iraqi Freedom: a pilot study. Pain Med. 2009;10:1237–45.
Asmundson GJ, Wright KD, Stein MB. Pain and PTSD symptoms in female veterans. Eur J Pain. 2004;8:345–50.
Mundy E, Blanchard E, Cirenza E, Gargiulo J, Maloy B, Blanchard C. Posttraumatic stress disorder in breast cancer patients following autologous bone marrow transplantation or conventional cancer treatments. Behav Res Ther. 2000;38:1015–27.
Scherwath A, Schirmer L, Kruse M, et al. Cognitive functioning in allogeneic hematopoietic stem cell transplantation recipients and its medical correlates: a prospective multicenter study. Psychooncology. 2013;22:1509–16.
Buccheri G, Ferrigno D, Tamburini M. Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer. 1996;32:1135–41.
Höcker A, Mehnert A. Posttraumatische Belastung bei Krebspatienten: Validierung der deutschen Version der Posttraumatic Stress Disorder Checklist–Civilian Version (PCL-C). Z Med Psychol. 2012;68:79.
Weathers FW, Huska JA, Keane TM. PCL-C for DSM-IV. Boston: National Center for PTSD – Behavioral Science Division; 1991.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23:129–38.
IBM Corporation. SPSS statistics for windows. Armonk, NY: IBM Corporation; 2011.
Andrykowski MA, Bishop MM, Hahn EA, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol. 2005;23:599–608.
Silberfarb PM, Oxman TE. The effects of cancer therapies on the central nervous system. Adv Psychosom Med. 1988;18:13.
Diez-Campelo M, Perez-Simon JA, Gonzalez-Porras JR, et al. Quality of life assessment in patients undergoing reduced intensity conditioning allogeneic as compared to autologous transplantation: results of a prospective study. Bone Marrow Transplant. 2004;34:729–38.
Gurevich M, Devins GM, Rodin GM. Stress response syndromes and cancer: conceptual and assessment issues. Psychosomatics. 2002;43:259–81.
Mehnert A, Berg P, Henrich G, Herschbach P. Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psychooncology. 2009;18:1273–80.
Breslau N. Gender differences in trauma and posttraumatic stress disorder. J Gend Specif Med. 2002;5:34–40.
National Center for PTSD. Using the PTSD Checklist for DSM-IV(PCL). 2014. http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/PCL-handout.pdf. Accessed 30 Nov 2015.
Yehuda R, Kahana B, Schmeidler J, Southwick SM, Wilson S, Giller EL. Impact of cumulative lifetime trauma and recent stress on current posttraumatic stress disorder symptoms in holocaust survivors. Am J Psychiatry. 1995;152:1815–8.
Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156:902–7.
Tjemsland L, Søreide JA, Malt UF. Posttraumatic distress symptoms in operable breast cancer III. Breast Cancer Res Treat. 1998;47:141–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The research was approved by the local ethics committees or the institutional review boards. Prior to participation, all patients provided written informed consent.
Funding
This study was funded by the José Carreras Leukämie-Stiftung e.V. (grant nos. DJCLS R 04/29pf and DJCLS R 07/37pf).
Conflict of interest
The funding source was not involved in any stage of the research process. The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Esser, P., Kuba, K., Scherwath, A. et al. Posttraumatic stress disorder symptomatology in the course of allogeneic HSCT: a prospective study. J Cancer Surviv 11, 203–210 (2017). https://doi.org/10.1007/s11764-016-0579-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0579-7