Abstract
Purpose
Cancer survivors’ needs around sexual concerns are often unmet. The primary objective of this systematic review was to examine the prevalence of and factors associated with patient-provider communication about sexual concerns in cancer.
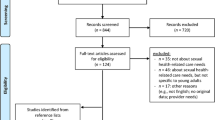
Methods
Using PRISMA guidelines, we searched PubMed/MEDLINE, PsychInfo, and CINAHL databases for peer-reviewed quantitative research papers (2000–2015) in cancer samples. Search terms across three linked categories were used (sexuality, communication, and cancer). The National Comprehensive Cancer Network (NCCN) Sexual Function Guidelines were used as a framework to categorize communication reported in each study.
Results
Twenty-nine studies from 10 countries (29 % in USA) were included. Studies assessed patients only (21), providers only (4), and both (4). Communication measures differed across studies and many lacked validity data. When reported by patients or providers, the average prevalence of discussing potential treatment effects on sexual function was 50 (60 % for men and 28 % for women) and 88 %, respectively. As reported by patients or providers, respectively, assessing patients’ sexual concerns (10 and 21 %) and offering treatments (22 and 17 %) were measured in fewer studies and were reported less frequently. Both patients and providers (28 and 32 %, respectively) reported a low prevalence of other non-specific communication. Greater prevalence of communication was associated with male patient gender and more years of provider experience.
Conclusions
Sexual issues go unaddressed for many cancer survivors, particularly women. Both patient and provider interventions are needed.
Implications for Cancer Survivors
Enhancing patient-provider communication about sexual concerns through evidence-based interventions could improve patient sexual function and quality of life.

Similar content being viewed by others
Notes
The term “discuss” was entered as a Boolean phrase as “discuss*” which searched for any word beginning with this item stem. The terms “sexual behavior,” “sexuality,” “communication,” and “neoplasms” were also included in relevant searches as a MESH term and/or subject heading in addition to their appearance in the title or abstract.
The Scheer study presented a prevalence rate using patient chart review (100 %) and patient self-report survey (53 %), both of which were included in the mean prevalence calculation.
References
Bober SL, Sanchez VV. Sexuality in adult cancer survivors: challenges and intervention. J Clin Oncol. 2012;30:3712–9.
Burwell SR, Case LD, Kaelin C, Avis NE. Sexual problems in younger women after breast cancer surgery. J Clin Oncol. 2006;24:2815–21.
Sadovsky R, Basson R, Krychman M, Morales AM, Schover L, Wang R, et al. Cancer and sexual problems. J Sex Med. 2010;7:349–73.
Syrjala KL, Roth-Roemer SL, Abrams JR, Scanlan JM, Chapko MK, Visser S, et al. Prevalence and predictors of sexual dysfunction in long-term survivors of marrow transplantation. J Clin Oncol. 1998;16:3148–57.
Taylor KL, Luta G, Miller AB, Church TR, Kelly SP, Muenz LR, et al. Long-term disease-specific functioning among prostate cancer survivors and noncancer controls in the prostate, lung, colorectal and ovarian cancer screening trial. J Clin Oncol. 2012;30:2768–75.
Carmack Taylor CL, Basen-Engquist K, Shinn EH, Bodurka DC. Predictors of sexual functioning in ovarian cancer patients. J Clin Oncol. 2004;22:881–9.
Ganz PA, Desmond KA, Belin TR, Meyerowitz BE, Rowland JH. Predictors of sexual health in women after a breast cancer diagnosis. J Clin Oncol. 1999;17:2371–80.
Kirk MC, Hudis CA. Insight into barriers against optimal adherence to oral hormonal therapy in women with breast cancer. Clin Breast Cancer. 2008;8:155–61.
Mortimer JE. Managing the toxicities of the aromatase inhibitors. Curr Opin Obstet Gynecol. 2010;22:56–60.
Bacon CG, Giovannucci E, Testa M, Glass TA, Kawachi I. The association of treatment-related symptoms with quality-of-life outcomes for localized prostate carcinoma patients. Cancer. 2002;94:862–71.
Nelson CJ, Mulhall JP, Roth AJ. The association between erectile dysfunction and depressive symptoms in men treated for prostate cancer. J Sex Med. 2011;8:560–6.
Reese JB, Shelby RA, Keefe FJ, Porter LS, Abernethy AP. Sexual concerns in cancer patients: a comparison of GI and breast cancer patients. Support Care Cancer. 2010;18:1179–89.
Ligibel JA, Denlinger CS. New NCCN guidelines® for survivorship care. J Natl Compr Canc Netw. 2013;11:640–4.
Lindau ST, Abramsohn EM, Baron SR, Florendo J, Haefner HK, Jhingran A, et al. Physical examination of the female cancer patient with sexual concerns: what oncologists and patients should expect from consultation with a specialist. CA Cancer J Clin. 2016;66:241–63.
Park ER, Norris RL, Bober SL. Sexual health communication during cancer care barriers and recommendations. Cancer J. 2009;15:74–7.
Hautamaki K, Miettinen M, Kellokumpu-Lehtinen PL, Aalto P, Lehto J. Opening communication with cancer patients about sexuality-related issues. Cancer Nurs. 2007;30:399–404.
Rasmusson EM, Plantin L, Elmerstig E. Did they think I would understand all that on my own? A questionnaire study about sexuality with Swedish cancer patients. Eur J Cancer Care (Engl). 2013;22:361–9.
East L, Hutchinson M. Moving beyond the therapeutic relationship: a selective review of intimacy in the sexual health encounter in nursing practice. J Clin Nurs. 2013;22:3568–76.
Dyer K, das Nair R. Why don’t healthcare professionals talk about sex? A systematic review of recent qualitative studies conducted in the United Kingdom. J Sex Med. 2013;10:2658–70.
Sporn NJ, Smith KB, Pirl WF, Lennes IT, Hyland KA, Park ER. Sexual health communication between cancer survivors and providers: how frequently does it occur and which providers are preferred? Psycho-Oncology. 2015;24:1167–73.
Lindau ST, Surawska H, Paice J, Baron SR. Communication about sexuality and intimacy in couples affected by lung cancer and their clinical-care providers. Psycho-Oncology. 2011;20:179–85.
Hordern AJ, Street AF. Communicating about patient sexuality and intimacy after cancer: mismatched expectations and unmet needs. Med J Aust. 2007;186:224–7.
Hordern AJ, Street AF. Let’s talk about sex: risky business for cancer and palliative care clinicians. Contemp Nurse. 2007;27:49–60.
Penson RT, Gallagher J, Gioiella ME, Wallace M, Borden K, Duska LA, et al. Sexuality and cancer: conversation comfort zone. Oncologist. 2000;5:336–44.
Stead ML, Brown JM, Fallowfield L, Selby P. Lack of communication between healthcare professionals and women with ovarian cancer about sexual issues. Br J Cancer. 2003;88:666–71.
Vermeer WM, Bakker RM, Stiggelbout AM, Creutzberg CL, Kenter GG, ter Kuile MM. Psychosexual support for gynecological cancer survivors: professionals’ current practices and need for assistance. Support Care Cancer. 2015;23:831–9.
Hill EK, Sandbo S, Abramsohn E, Makelarski J, Wroblewski K, Wenrich ER, et al. Assessing gynecologic and breast cancer survivors’ sexual health care needs. Cancer. 2011;117:2643–51.
Flynn KE, Reese JB, Jeffery DD, Abernethy AP, Lin L, Shelby RA, et al. Patient experiences with communication about sex during and after treatment for cancer. Psycho-Oncology. 2012;21:594–601.
Ussher JM, Perz J, Gilbert E, Wong WK, Mason C, Hobbs K, et al. Talking about sex after cancer: a discourse analytic study of health care professional accounts of sexual communication with patients. Psychol Health. 2013;28:1370–90.
Traa MJ, De Vries J, Roukema JA, Rutten HJ, Den Oudsten BL. The sexual health care needs after colorectal cancer: the view of patients, partners, and health care professionals. Support Care Cancer. 2014;22:763–72.
McClelland SI, Holland KJ, Griggs JJ. Vaginal dryness and beyond: the sexual health needs of women diagnosed with metastatic breast cancer. J Sex Res. 2015;52:604–16.
Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–3.
Regan TW, Lambert SD, Kelly B, Falconier M, Kissane D, Levesque JV. Couples coping with cancer: exploration of theoretical frameworks from dyadic studies. Psychooncology. 2015;24:1605–17.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Survivorship. National Comprehensive Cancer Network, Inc.; 2015.
Haywood Jr C, Beach MC, Lanzkron S, Strouse JJ, Wilson R, Park H, et al. A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. J Natl Med Assoc. 2009;101:1022–33.
Segal JB, Strouse JJ, Beach MC, Haywood C, Witkop C, Park HS et al. Hydroxyurea for the Treatment of Sickle Cell Disease. Evidence Report/Technology Assessment No. 165. Rockville, MD: Prepared by Johns Hopkins University Evidence-based Practice Center under contract No. 290-02-0018; February 2008.
Hendren SK, Swallow CJ, Smith A, Lipa JE, Cohen Z, MacRae HM, et al. Complications and sexual function after vaginectomy for anorectal tumors. Dis Colon Rectum. 2007;50:810–6.
Lewis PE, Sheng M, Rhodes MM, Jackson KE, Schover LR. Psychosocial concerns of young African American breast cancer survivors. J Psychosoc Oncol. 2012;30:168–84.
Khoo SB. Impact of cancer on psychosexuality: cultural perspectives of Asian women. Int J Nurs Pract. 2009;15:481–8.
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF et al. SEER Cancer Statistics Review, 1975-2013, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2013/, based on November 2015 SEER data submission, posted to the SEER web site, April 2016.
Scheer AS, O’Connor AM, Chan BP, Moloo H, Poulin EC, Mamazza J, et al. The myth of informed consent in rectal cancer surgery: what do patients retain? Dis Colon Rectum. 2012;55:970–5.
Boyd BG, McCallum SW, Lewis RW, Terris MK. Assessment of patient concern and adequacy of informed consent regarding infertility resulting from prostate cancer treatment. Urology. 2006;68:840–4.
Cox A, Jenkins V, Catt S, Langridge C, Fallowfield L. Information needs and experiences: an audit of UK cancer patients. Eur J Oncol Nurs. 2006;10:263–72.
Errihani H, Elghissassi I, Mellas N, Belbaraka R, Messmoudi M, Kaikani W. Impact of cancer on sexuality: how is the Moroccan patient affected? Sexologies: Eur J Sexology Sex Health / Rev Eur Sex Sante Sex. 2010;19:92–8.
Forbat L, White I, Marshall-Lucette S, Kelly D. Discussing the sexual consequences of treatment in radiotherapy and urology consultations with couples affected by prostate cancer. BJU Int. 2012;109:98–103.
Hendren SK, O’Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ, et al. Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg. 2005;242:212–23.
Huang LL, Pu J, Liu LH, Du XB, Wang J, Li JY, et al. Cancer department nurses’ attitudes and practices in response to the sexual issues of pelvic radiation patients: a survey in Sichuan. China Contemp Nurse. 2013;43:146–51.
Kunneman M, Marijnen CA, Rozema T, Ceha HM, Grootenboers DA, Neelis KJ, et al. Decision consultations on preoperative radiotherapy for rectal cancer: large variation in benefits and harms that are addressed. Br J Cancer. 2015;112:39–43.
Lemieux L, Kaiser S, Pereira J, Meadows LM. Sexuality in palliative care: patient perspectives. Palliat Med. 2004;18:630–7.
Lindau ST, Gavrilova N, Anderson D. Sexual morbidity in very long term survivors of vaginal and cervical cancer: a comparison to national norms. Gynecol Oncol. 2007;106:413–8.
Mohamed NE, Chaoprang Herrera P, Hudson S, Revenson TA, Lee CT, Quale DZ, et al. Muscle invasive bladder cancer: examining survivor burden and unmet needs. J Urol. 2014;191:48–53.
Scanlon M, Blaes A, Geller M, Majhail NS, Lindgren B, Haddad T. Patient satisfaction with physician discussions of treatment impact on fertility, menopause and sexual health among pre-menopausal women with cancer. J Cancer. 2012;3:217–25.
Southard NZ, Keller J. The importance of assessing sexuality: a patient perspective. Clin J Oncol Nurs. 2009;13:213–7.
Ussher JM, Perz J, Gilbert E. Information needs associated with changes to sexual well-being after breast cancer. J Adv Nurs. 2013;69:327–37.
Vermeer WM, Bakker RM, Kenter GG, de Kroon CD, Stiggelbout AM, ter Kuile MM. Sexual issues among cervical cancer survivors: how can we help women seek help? Psycho-Oncology. 2015;24:458–64.
White ID, Allan H, Faithfull S. Assessment of treatment-induced female sexual morbidity in oncology: is this a part of routine medical follow-up after radical pelvic radiotherapy? Br J Cancer. 2011;105:903–10.
Hilarius DL, Kloeg PH, Gundy CM, Aaronson NK. Use of health-related quality-of-life assessments in daily clinical oncology nursing practice: a community hospital-based intervention study. Cancer. 2008;113:628–37.
Gilbert E, Perz J, Ussher JM. Talking about sex with health professionals: the experience of people with cancer and their partners. Eur J Cancer Care. 2016;25:280–93.
Krouwel EM, Nicolai MP, van Steijn-van Tol AQ, Putter H, Osanto S, Pelger RC, et al. Addressing changed sexual functioning in cancer patients: a cross-sectional survey among Dutch oncology nurses. Eur J Oncol Nurs. 2015;19:707–15.
Kedde H, van de Wiel HB, Weijmar Schultz WC, Wijsen C. Sexual dysfunction in young women with breast cancer. Support Care Cancer. 2013;21:271–80.
Oskay U, Can G, Basgol S. Discussing sexuality with cancer patients: oncology nurses attitudes and views. Asian Pac J Cancer Prev. 2014;15:7321–6.
Silva Lara LA, de Andrade JM, Consolo FD, Salata Romao APM. Women’s poorer satisfaction with their sex lives following gynecologic cancer treatment. Clin J Oncol Nurs. 2012;16:273–7.
Chorost MI, Weber TK, Lee RJ, Rodriguez-Bigas MA, Petrelli NJ. Sexual dysfunction, informed consent and multimodality therapy for rectal cancer. Am J Surg. 2000;179:271–4.
Shepherd HL, Barratt A, Trevena LJ, McGeechan K, Carey K, Epstein RM, et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: a cross-over trial. Patient Educ Couns. 2011;84:379–85.
Mercadante S, Vitrano V, Catania V. Sexual issues in early and late stage cancer: a review. Support Care Cancer. 2010;18:659–65.
Ussher JM, Perz J, Gilbert E. Perceived causes and consequences of sexual changes after cancer for women and men: a mixed method study. BMC Cancer. 2015;15:268.
Ferreira SM, Gozzo Tde O, Panobianco MS, Santos MA, Almeida AM. Barriers for the inclusion of sexuality in nursing care for women with gynecological and breast cancer: perspective of professionals. Rev Lat Am Enfermagem. 2015;23:82–9.
Julien JO, Thom B, Kline NE. Identification of barriers to sexual health assessment in oncology nursing practice. Oncol Nurs Forum. 2010;37:E186–90.
Reese JB, Haythornthwaite JA. Importance of sexuality in colorectal cancer: predictors, changes, and response to an intimacy enhancement intervention. Support Care Cancer. 2016;24:4309–17.
Arora NK, Jensen RE, Sulayman N, Hamilton AS, Potosky AL. Patient-physician communication about health-related quality-of-life problems: are non-Hodgkin lymphoma survivors willing to talk? J Clin Oncol. 2013;31:3964–70.
Melisko ME, Goldman M, Rugo HS. Amelioration of sexual adverse effects in the early breast cancer patient. J Cancer Surviv. 2010;4:247–55.
Bennett MI, Bagnall A-M, Closs SJ. How effective are patient-based educational interventions in the management of cancer pain? Systematic review and meta-analysis. Pain. 2009;143:192–9.
Berry DL, Blumenstein BA, Halpenny B, Wolpin S, Fann JR, Austin-Seymour M, et al. Enhancing patient-provider communication with the electronic self-report assessment for cancer: a randomized trial. J Clin Oncol. 2011;29:1029–35.
Hordern A, Grainger M, Hegarty S, Jefford M, White V, Sutherland G. Discussing sexuality in the clinical setting: the impact of a brief training program for oncology health professionals to enhance communication about sexuality. Asia Pac J Clin Oncol. 2009;5:270–7.
Vadaparampil ST, Gwede CK, Meade C, Kelvin J, Reich RR, Reinecke J et al. ENRICH: A promising oncology nurse training program to implement ASCO clinical practice guidelines on fertility for AYA cancer patients. Patient Educ Couns. 2016.
Zill JM, Christalle E, Müller E, Härter M, Dirmaier J, Scholl I. Measurement of physician-patient communication—a systematic review. PLoS One. 2014;9:e112637.
Bober SL, Reese JB, Barbera L, Bradford A, Carpenter KM, Goldfarb S, et al. How to ask and what to do: a guide for clinical inquiry and intervention regarding female sexual health after cancer. Curr Opin Support Palliat Care. 2016;10:44–54.
Schover LR. Counseling cancer patients about changes in sexual function. Oncology (Williston Park). 1999;13:1585–91.
Acknowledgments
Jennifer Barsky Reese was supported by a Mentored Research Scholar Grant (MRSG-14-031-01-CPPB) from the American Cancer Society and by P30 CA006927 from the National Cancer Institute. The funding agencies had no role in the conduct of this study. We wish to thank Karenann Jurecki and Beth Lewis in the Fox Chase Talbot Research Library for their assistance with the searches.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to report
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 42 kb)
Rights and permissions
About this article
Cite this article
Reese, J.B., Sorice, K., Beach, M.C. et al. Patient-provider communication about sexual concerns in cancer: a systematic review. J Cancer Surviv 11, 175–188 (2017). https://doi.org/10.1007/s11764-016-0577-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0577-9