Abstract
Purpose
Little population-based research has been done on social, economic, and environmental factors affecting quality of life (QOL) among long-term cancer survivors. This research assesses the impact of disease and nondisease factors on QOL among long-term survivors of cervical cancer.
Methods
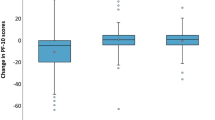
In a collaborative, observational study, data were obtained from cancer registries, interviews, and self-administered questionnaires. Comparisons of QOL were made between women with cervical cancer histories and women from the general population. A total of 715 women 4–28 years postdiagnosis were identified from cancer registries in Connecticut (N = 208), Detroit Metropolitan Area (N = 211), New Mexico (N = 197), and Hawaii (N = 99). QOL was measured according to four SF-36 dimensions—physical functioning, social functioning, bodily pain, and general health status.
Results
Means on SF-36 measures among women with cervical cancer histories were close to or higher than women in the general population. In a multiple regression analysis, economic disadvantage negatively predicted physical functioning (B = −13.4, SE = 2.1), social functioning (B = −13.2, SE = 2.4), bodily pain (B = −12.6, SE = 2.5), and general health (B = −12.8, SE = 2.1). Residence in New Mexico negatively predicted several QOL dimensions. No impact of race was detected when income was controlled. Disease stage did not predict QOL.
Conclusions
Cervical cancer does not generally reduce QOL among long-term survivors. Economic disadvantage and residential location affect QOL through mechanisms yet to be determined.
Implications for Cancer Survivors
Women diagnosed with cervical cancer have good prospects for high quality of life; socioeconomic status strongly affects quality of life over the long term.
Similar content being viewed by others
References
Williams DR, Mohammed SA, Leavell J. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann NY Acad Sci. 2010;1186:69–101.
Kaur JS, Coe K, Rowland J. Enhancing life after cancer in diverse communities. Cancer. 2012;118(21):5366–73.
Moadel AB, Morgan CM, Dutcher J. Psychosocial needs assessment among an underserved, ethnically diverse cancer patient population. Cancer. 2007;109(Supplement 2):446–54.
American Cancer Society. Cancer facts and figures. Atlanta: American Cancer Society; 2013.
De Moor JS, Marietto AB, Parry C, Alfano MA. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22(4):651–70.
Weaver KE, Forsythe LP, Reeve BB, et al. Mental and physical health-related quality of life among U.S. cancer survivors: population estimates from the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2012;21(11):2108–17.
Richardson LC, Wingo PA, Zack MM, et al. Health-related quality of life in cancer survivors between ages 20 and 64 years: population-based estimates from the Behavioral Risk Factor Surveillance System. Cancer. 2008;112(6):1380–9.
Matthews AK, Tejeda S, Johnson TP, et al. Correlates of quality of life among Africa-American and White cancer survivors. Cancer Nurs. 2012;35(5):355–64.
Ashing-Giwa KT, Lim J. Examining the impact of socioeconomic status and socioecologic stress on physical and mental health quality of life among breast cancer survivors. Oncol Nurs Forum. 2009;36:79–88.
Ashing-Giwa KT, Tejero JS, Kim J, et al. Cervical cancer survivorship in a population based sample. Gynecol Oncol. 2009;112:358–64.
Luckett T, Goldstein D, Butlow PN, et al. Psychological morbidity and quality of life of ethnic minority patients with cancer: a systematic review and meta-analysis. Lancet Oncol. 2011;12(13):1240–8.
Powe BD, Hamilton J, Hancock N, et al. Quality of life of African-American Cancer Survivors: a review of the literature. Cancer. 2007;109(Issuer Supplement 2):435–45.
Davis RM, Cullin JW, Miller LS, Titus M. Physical rehabilitation. In: Haskell WB, editor. Cancer treatment. Philadelphia: Saunders; 1986. p. 940–5.
Dobkin PL, Morrow GR. Long-term side effects in patients who have been treated successfully for cancer. J Psychosoc Oncol. 1986;3:23–51.
Poplack DG, Brouwers P. Late CNS sequelae in long-term survivors of childhood leukemia. Proceedings of the fifth national conference on human values and cancer-1987. Atlanta: American Cancer Society; 1987. p. 35–41.
Bonica JJ. Importance of the problem. In: Bonica JJ, Ventafridda V, editors. Advances in pain research and therapy. New York: Raven; 1979.
Daut RL, Cleeland CS. The prevalence and severity of pain in cancer. Cancer. 1982;50:1913–8.
Coyle N, Foley K. Pain in patients with cancer: profile of patients and common pain syndromes. Semin Oncol Nurs. 1985;1:93–9.
Chapman CR, Syrjala K, Sargur M. Pain as a manifestation of cancer treatment. Semin Oncol Nurs. 1985;1:100–8.
Derogatis LR, Morrow GR, Fetting J, et al. The prevalence of psychiatric disorders among cancer patients. JAMA. 1983;249:751–7.
Kornblith AB, Anderson J, Cella DF, et al. Hodgkin disease survivors at increased risk for problems in psychosocial adaptation. Cancer. 1992;70:2214–24.
Shands ME, Lewis F, Zahlis EH. Mother and child interactions about the mother’s breast cancer: an interview study. Oncol Nurs Forum. 2000;27:77–85.
Lewis FM, Hammond MA. Psychosocial adjustment of the family to breast cancer: a longitudinal study. J Am Med Wom Assoc. 1996;47:194–200.
Yabroff KR, Lawrence FW, Clauser S, et al. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst. 2004;96:1322–30.
Bradley CJ, Bednarek HL, Newmark D. Breast cancer survival, work, and earnings. J Health Econ. 2003;21:757–9.
Greenwald HP, Dirks SJ, Borgatta EF, et al. Work disability among cancer patients. Soc Sci Med. 1989;29:1253–9.
Corney R, Everett H, Howells A, et al. The care of patients undergoing surgery for gynecological cancer: the need for information, emotional support and counseling. J Adv Nurs. 1992;17:667–71.
Bukovic D, Strinie T, Habek M, et al. Sexual life after cervical carcinoma. Coll Anthropol. 2003;27:173–80.
Juraskova I, Butnow P, Robertson R. Post-treatment sexual adjustment following cervical and endometrial cancer: a qualitative insight. Psycho-Oncol. 2003;12:267–79.
Jensen PT, Groenvold M, Klee MC, et al. Early-stage cervical carcinoma, radical hysterectomy, and sexual function. Cancer. 2004;100:97–106.
Elit L, Esplem MJ, Butler K, et al. Quality of life and psychosexual adjustment after prophylactic oophrectomy for a family history of ovarian cancer. Fam Cancer. 2001;1:149–56.
Robson M, Hensley M, Barakat R, et al. Quality of life in women at risk for ovarian cancer who have undergone risk-reducing oophrectomy. Gynecol Oncol. 2003;89:281–7.
Roussis NF, Waltrous L, Kerr A, et al. Sexual response in the patients after hysterectomy, total abdominal versus supracervical versus vaginal procedure. Am J Obstet Gynecol. 2004;190:1427–8.
Herzog TJ, Wright JD. The impact of cervical cancer on quality of life—the components and means for management. Gynecol Oncol. 2007;107:572–7.
Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112(Issue Supplement 11):2577–92.
Ganz PA. Survivorship: adult cancer survivors. Prim Care. 2009;36:721–41.
Mettlin CJ, Menck HR, Winchester DP, et al. A comparison of breast, colorectal, lung, and prostate cancers reported to the National Cancer Data Base and the Surveillance, Epidemiology, and End Results Program. Cancer. 1997;79(10):2052–61.
Zippin C, Lum D, Hankey BF. Completeness of hospital cancer case reporting from the SEER Program of the National Cancer Institute. Cancer. 1995;76:2343–50.
Greenwald HP, McCorkle R, Fennie K. Health status and adaptation among long-term cervical cancer survivors. Gynecol Oncol. 2008;111:449–54.
Bartoces MG, Severson RK, Rusin BA, et al. Quality of life and self-esteem of long-term survivors of invasive and noninvasive cervical cancer. J Womens Health. 2009;18(5):655–61.
McHorney CA, Kosinski MA, Ware JE. Comparisons of the costs and quality of norms for the SF-36 health survey collected by mail versus telephone interview: results from a national survey. Med Care. 1994;32:551–67.
National Center for Health Statistics. Health, United States, 1995. Hyattsville: Public Health Service; 1996. http://www.cdc.gov/nchs/data/hus/hus95. Accessed 23 Dec 2013.
National Center for Health Statistics. Health, United States, 2005. Hyattsville: Public Health Service; 2006. http://www.cdc.gov/nchs/data/hus/hus05. Accessed 23 Dec 2013.
Ware JE, Sherbourne CD. The MOS 36-item short form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
McHorney CA, Ware JE, Rachel Lu JF, et al. The MOS-36 Short Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66.
Ware JE, Kosinski MA, Gandek MA. SF-36 health survey: manual and interpretation guide. Boston: New England Medical Center, The Health Institute; 1993.
Altekruse SF, Kosary CL, Krapcho M, et al., editors. SEER Cancer Statistics Review, 1975-2008. Bethesda: National Cancer Institute; 2008. http://seer.cancer.gov/csr/1975_2008/. Accessed 17 Jul 2011.
Greenwald HP, McCorkle R. Remedies and life changes among invasive cervical cancer survivors. Urol Nurs. 2007;27(1):47–53.
Bardwell WA, Natarajan L, Dimsdale JE, et al. Objective cancer-related variables are not associated with depressive symptoms in women treated for early-stage breast cancer. J Clin Oncol. 2006;24:2420–7.
Scheier MF, Helgeson VS. Really, disease doesn’t matter? A commentary on correlates of depressive symptoms in women treated for early-stage breast cancer. J Clin Oncol. 2006;24:2407–8.
Do DP, Finch BK, Basturo R, et al. Does place explain racial health disparities? Quantifying the contribution of residential context to the Black/White health gap in the United States. Soc Sci Med. 2008;67:1258–68.
Weaver KE, Geiger AM, Lu L, Case LD. Rural-urban disparities in health status among US cancer survivors. Cancer. 2013;119(5):1050–7.
Sathyanarayanan S, Brooks AJ, Hagen SE, et al. Multilevel analysis of the physical health perception of employees: community and individual factors. Am J Health Promot. 2012;26(5):e126–36.
Barger SD, Donoho CJ, Wayment HA. The relative contributions of race/ethnicity, socioeconomic status, health, and social relationships to life satisfaction in the United States. Qual Life Res. 2009;18(2):179–89.
Yang Y. Social inequalities and happiness in the United States: 1972–2004: an age-period cohort analysis. Am Sociol Rev. 2008;73(2):204–26.
Acknowledgments
This research was supported by the following grants and contracts: SEER Special Studies Connecticut Department of Health 2001-345, NO1-PC-65064, NO1-PC-CN 77001, and NO1-PC-67007.
Conflicts of interest
None of the authors of this article have any conflict of interest, financial or otherwise.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Greenwald, H.P., McCorkle, R., Baumgartner, K. et al. Quality of life and disparities among long-term cervical cancer survivors. J Cancer Surviv 8, 419–426 (2014). https://doi.org/10.1007/s11764-014-0352-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0352-8