Abstract
Objective
We examined cases in which delirium developed after thoracic surgery under general anesthesia at our hospital to determine the predictive factors for postoperative delirium, as well as the perioperative findings in cases showing postoperative delirium.
Methods
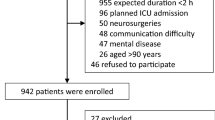
This retrospective study included 1674 patients who underwent surgery under general anesthesia at our hospital between 2012 and 2022, A psychiatrist diagnosed postoperative delirium using the Confusion Assessment Method.
Results
There were 99 (5.9%) patients with postoperative delirium in our study, including 85 (86%) men, of whom 31 (31%) had a history of cerebrovascular disease. The incidence of postoperative delirium in patients aged > 80 years was 20% (36/182). The postoperative delirium group showed significantly longer hospital stays and more frequent postoperative complications than the group without postoperative delirium. In univariate analysis, age ≥ 80 years, male sex, history of cerebrovascular disease, hypertension, history of atrial fibrillation, and history of smoking were identified as significant factors, while multivariate analysis identified age ≥ 80 years, male sex, history of cerebrovascular disease, hypertension, and history of smoking as significant factors (odds ratios = 5.15, 2.04, 3.10, 1.67, and 2.36, respectively). In the 169 cases with none of these five factors, the postoperative delirium risk was 0% (0/169).
Conclusions
In patients undergoing thoracic surgery, predictive factors for postoperative delirium include age ≥ 80 years, male sex, history of cerebrovascular disease, hypertension, and smoking history. The findings also indicate that patients with these risk factors may require psychiatric consultation before surgery.



Similar content being viewed by others
References
Brand CA, Sundararajan V. A 10-year cohort study of the burden and risk of in-hospital falls and fractures using routinely collected hospital data. Qual Saf Health Care. 2010;19: e51.
Edlund A, Lundström M, Karlsson S, Brännström B, Bucht G, Gustafson Y. Delirium in older patients admitted to general internal medicine. J Geriatr Psychiatry Neurol. 2006;19:83–90.
Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168:27–32.
Kamiya M, Aoyama T, Kano K, Murakawa M, Kazama K, Atsumi Y, et al. Risk factors for postoperative delirium after gastrointestinal surgery—using randomized Phase II trial data. Ann Cancer Res Ther. 2018;26:95–100.
Chen H, Mo L, Hu H, Ou Y, Luo J. Risk factors of postoperative delirium after cardiac surgery: a meta-analysis. J Cardiothorac Surg. 2021;16:113.
Rong X, Ding Z-C, Yu H, Yao S-Y, Zhou Z-K. Risk factors of postoperative delirium in the knee and hip replacement patients: a systematic review and meta-analysis. J Orthop Surg Res. 2021;16:76.
Yildizeli B, Ozyurtkan MO, Batirel HF, Kuşcu K, Bekiroğlu N, Yüksel M. Factors associated with postoperative delirium after thoracic surgery. Ann Thorac Surg. 2005;79:1004–9.
Marcantonio ER. Delirium in hospitalized older adults. N Engl J Med. 2017;377:1456–66.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–8.
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive care delirium screening checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27:859–64.
Gusmao-Flores D, Figueira Salluh JI, Chalhub RA, Quarantini LC. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care. 2012;16(4):R115.
Janssen TL, Steyerberg EW, Faes MC, Wijsman JH, Gobardhan PD, Ho GH, et al. Risk factors for postoperative delirium after elective major abdominal surgery in elderly patients: a cohort study. Int J Surg. 2019;71:29–35.
Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383:911–22.
American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. J Am Geriatr Soc. 2015;63:142–50.
National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Version5.0.2017. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50.
Raz N, Rodrigue KM. Differential aging of the brain: patterns, cognitive correlates and modifiers. Neurosci Biobehav Rev. 2006;30:730–48.
Wilson RS, Segawa E, Boyle PA, Bennett DA. Influence of late-life cognitive activity on cognitive health. Neurology. 2012;78:1123–9.
Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012;11:1006–12.
Marcantonio ER, Goldman L, Mangione CM, Ludwig LE, Muraca B, Haslauer CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994;271:134–9.
Mangoni AA, Jackson SHD. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57:6–14.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47:30–9.
Holtzman RE, Rebok GW, Saczynski JS, Kouzis AC, Wilcox Doyle K, Eaton WW. Social network characteristics and cognition in middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci. 2004;59:P278-284.
Park DC, Reuter-Lorenz P. The adaptive brain: aging and neurocognitive scaffolding. Annu Rev Psychol. 2009;60:173–96.
Ziegler G, Dahnke R, Jäncke L, Yotter RA, May A, Gaser C. Brain structural trajectories over the adult lifespan. Hum Brain Mapp. 2012;33:2377–89.
Brinton RD. The healthy cell bias of estrogen action: mitochondrial bioenergetics and neurological implications. Trends Neurosci. 2008;31:529–37.
Vedder LC, Bredemann TM, McMahon LL. Estradiol replacement extends the window of opportunity for hippocampal function. Neurobiol Aging. 2014;35:2183–92.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health consequences of smoking—50 years of progress: a report of the surgeon general. Atlanta Centers for Disease Control and Prevention (US); 2014. https://www.ncbi.nlm.nih.gov/books/NBK179276/
Rudolph JL, Marcantonio ER. Review articles: postoperative delirium: acute change with long-term implications. Anesth Analg. 2011;112:1202–11.
Acknowledgements
We would like to thank Editage (www.editage.com) for the English language editing.
Funding
This study was supported in part by a Grant-in-Aid for Special Research in Subsidies for the ordinary expenses of private schools from The Promotion and Mutual Aid Corporation for Private Schools of Japan.
Author information
Authors and Affiliations
Contributions
T. Y., H. I., M. S., K. K., T. M., K. T., E. K., and K. S. conceived and planned the experiments. T. Y., K. K. and H. I. planned and performed the simulations. T. Y., M. S., K. K., and H. I. contributed to sample preparation. T. Y., T. M., K. T., E. K., and K. S. interpreted the results. T. Y. took the lead in writing the manuscript. All the authors provided critical feedback and helped shape the research, analysis, and manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yaguchi, T., Ichinokawa, H., Kirino, E. et al. Predictive factors for postoperative delirium in thoracic surgery. Gen Thorac Cardiovasc Surg (2024). https://doi.org/10.1007/s11748-024-02014-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11748-024-02014-0