Abstract
Background
Despite the growing popularity of robotically assisted mitral repair, robotically assisted tricuspid repair has not been widely adopted. We assessed the safety and feasibility of robotic tricuspid annuloplasty with continuous sutures for tricuspid regurgitation (TR).
Methods and results
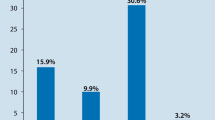
We studied consecutive 68 patients (median age, 74 years) with secondary TR who underwent tricuspid annuloplasty using continuous sutures with (n = 61) and without mitral valve repair (n = 7) from 2018 to 2021. Robotic tricuspid annuloplasty consists of continuous sutures with flexible prosthetic band to the tricuspid annulus using two V-Loc barbed sutures (Medtronic Inc., Minneapolis, MN). Concomitant maze procedure was performed in 45 (66%) patients. Robotic tricuspid annuloplasty with continuous sutures was successfully performed. There was no in-hospital or 30-day mortality; 65 patients (96%) did not experience major surgery-related complications. Preoperatively, the TR grade was mild in 20 (29%) patients and mildly higher in 48 (71%). Postoperatively, the TR severity significantly improved, with TR grade mildly higher in 9% at hospital discharge and 7% at 1-year follow-up (p < 0.001). The 1-year and 2-year freedom rates from heart failure were 98% and 95%, respectively.
Conclusions
Robotic tricuspid annuloplasty with continuous sutures is safe and feasible alone or concomitant with mitral valve repair. It offered sustained improvement in TR severity and might prevent heart failure readmission.




Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Izumi C, Miyake M, Takahashi S, Matsutani H, Hashiwada S, Kuwano K, et al. Progression of isolated tricuspid regurgitation late after left-sided valve surgery: clinical features and mechanisms. Circ J. 2011;75:2902–7.
Lee H, Sung K, Kim WS, Lee YT, Park SJ, Carriere KC, et al. Clinical and hemodynamic influences of prophylactic tricuspid annuloplasty in mechanical mitral valve replacement. J Thorac Cardiovasc Surg. 2016;151:788–95.
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, et al. 2020 ACC/AHA Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143:e72–227.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg. 2021;60:727–800.
Lewis CT, Stephens RL, Tyndal CM, Cline JL. Concomitant robotic mitral and tricuspid valve repair: technique and early experience. Ann Thorac Surg. 2014;97:782–7.
Kawamoto N, Fukushima S, Shimahara Y, Yamasaki T, Matsumoto Y, Yamashita K, et al. Benefit and risk of minimally invasive mitral valve repair for type II dysfunction—propensity score matched comparison. Circ J. 2018;83:224–31.
Toya T, Fujita T, Fukushima S, Shimahara Y, Kume Y, Yamashita K, et al. Efficacy of regional saturation of oxygen monitor using near-infrared spectroscopy for lower limb ischemia during minimally invasive cardiac surgery. J Artif Organs. 2018;21:420–6.
Kakuta T, Fukushima S, Shimahara Y, Yajima S, Tadokoro N, Minami K, et al. Early results of robotically assisted mitral valve repair in a single institution: report of the first 100 cases. Gen Thorac Cardiovasc Surg. 2020;68:1079–85.
Watanabe G, Ishikawa N. Use of barbed suture in robot-assisted mitral valvuloplasty. Ann Thorac Surg. 2015;99:343–5.
Dreyfus GD, Corbi PJ, Chan KM, Bahrami T. Secondary tricuspid regurgitation of dilatation: which should be the criteria for surgical repair? Ann Thorac Surg. 2005;79:127–32.
Carpentier A, Deloche A, Hanania G, Forman J, Sellier P, Piwnica A, et al. Surgical management of acquired tricuspid valve disease. J Thorac Cardiovasc Surg. 1974;67:53–65.
Sakon Y, Murakami T, Fujii H, Takahashi Y, Morisaki A, Yamane K, et al. New insight into tricuspid valve anatomy from 100 hearts to reappraise annuloplasty methodology. Gen Thorac Cardiovasc Surg. 2019;67:758–64.
Hata H, Fujita T, Miura S, Shimahara Y, Kume Y, Matsumoto Y, et al. Long- term outcomes of suture vs ring tricuspid annuloplasty for functional tricuspid regurgitation. Circ J. 2017;81:1432–8.
Acknowledgements
We would like to thank Gina F from Enago (www.enago.jp) for the English language review.
Funding
This research did not receive any specific graft from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Writing: KN. Critical review and revision: all authors. Final approval of the article: all authors. Accountability for all aspects of the work: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
IRB information
Reporting was approved by NCVC institutional review board. Reference number is M30-026-8. https://www.ncvc.go.jp/hospital/wp-content/uploads/sites/2/M30-026-8_1.pdf
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Noda, K., Fukushima, S., Kakuta, T. et al. Short- and Midterm outcomes of modified robotic tricuspid annuloplasty for secondary tricuspid regurgitation. Gen Thorac Cardiovasc Surg 71, 692–699 (2023). https://doi.org/10.1007/s11748-023-01950-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-023-01950-7