Abstract
Background
Lung segmentectomy is an option for the treatment of noninvasive or minimally invasive lung cancer. For tumors located in the left upper division (LUD), LUD trisegmentectomy (S1+2 + S3) is frequently performed as a sublobar resection because of its technical simplicity. However, the differences in surgical outcomes between simple and complex segmentectomies remain unclear.
Methods
We compared the surgical outcomes and frequency of postoperative complications of LUD trisegmentectomy (simple group) with those of complex segmentectomy (other than LUD trisegmentectomy; complex group) for pulmonary lesions using three-dimensional computed tomography between 2010 and 2021.
Results
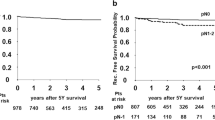
In total, 118 patients were included: 65 in the simple group and 53 in the complex group (S1+2: 25, S3: 15, others: 13). There were no significant differences in surgical time or duration of postoperative chest drainage. However, the blood loss volume was significantly smaller in the complex group than in the simple group (12 vs. 36 mL, p = 0.023), and major complications tended to occur less frequently in the complex group than in the simple group (3.8 vs. 13.8%, p = 0.061). Among patients who underwent intentional segmentectomy for primary lung cancer (n = 61), major complications were significantly less common in the complex group (p = 0.006).
Conclusions
Complex segmentectomy can be performed safely under the guidance of three-dimensional CT. Complex segmentectomy itself is not a risk factor for postoperative complications when the intersegmental planes are sufficiently recognized and accurately cut.




Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- AL:
-
Air leakage
- CT:
-
Computed tomography
- LUD:
-
Left upper division
- NSCLC:
-
Non-small cell lung cancer
References
Handa Y, Tsutani Y, Mimae T, Tasaki T, Miyata Y, Okada M. Surgical outcomes of complex versus simple segmentectomy for stage i non-small cell lung cancer. Ann Thorac Surg. 2019;107(4):1032–9.
Suzuki K, Saji H, Aokage K, et al. Comparison of pulmonary segmentectomy and lobectomy: safety results of a randomized trial. J Thorac Cardiovasc Surg. 2019;158(3):895–907.
Miyasaka Y, Oh S, Takahashi N, Takamochi K, Suzuki K. Postoperative complications and respiratory function following segmentectomy of the lung—comparison of the methods of making an inter-segmental plane. Interact Cardiovasc Thorac Surg. 2011;12(3):426–9.
Koike Y, Hattori A, Matsunaga T, Takamochi K, Oh S, Suzuki K. Postsurgical residual lung complications following left upper trisegmentectomy. Eur J Cardiothorac Surg. 2020;57(3):472–7.
Nakazawa S, Shimizu K, Kawatani N, et al. Right upper lobe segmentectomy guided by simplified anatomic models. JTCVS Tech. 2020;4:288–97.
Nakazawa S, Shimizu K, Mogi A, Kuwano H. Vats segmentectomy: past, present, and future. Gen Thorac Cardiovasc Surg. 2018;66(2):81–90.
Ohtaki Y, Shimizu K. Anatomical thoracoscopic segmentectomy for lung cancer. Gen Thorac Cardiovasc Surg. 2014;62(10):586–93.
Yajima T, Shimizu K, Mogi A, et al. Pulmonary artery compression facilitates intersegmental border visualization. Ann Thorac Surg. 2019;108(2):e141–3.
Shimizu K, Nagashima T, Yajima T, et al. Thoracoscopic medial-basal segment segmentectomy. Ann Thorac Surg. 2017;104(5):e403–6.
Nagashima T, Shimizu K, Ohtaki Y, et al. An analysis of variations in the bronchovascular pattern of the right upper lobe using three-dimensional CT angiography and bronchography. Gen Thorac Cardiovasc Surg. 2015;63(6):354–60.
Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg. 2011;141(3):678–82.
Dai C, Shen J, Ren Y, et al. Choice of surgical procedure for patients with non-small-cell lung cancer ≤ 1 cm or > 1 to 2 cm among lobectomy, segmentectomy, and wedge resection: a population-based study. J Clin Oncol. 2016;34(26):3175–82.
Razi SS, Nguyen D, Villamizar N. Lobectomy does not confer survival advantage over segmentectomy for non-small cell lung cancer with unsuspected nodal disease. J Thorac Cardiovasc Surg. 2020;159(6):2469-2483 e2464.
Hwang Y, Kang CH, Kim HS, Jeon JH, Park IK, Kim YT. Comparison of thoracoscopic segmentectomy and thoracoscopic lobectomy on the patients with non-small cell lung cancer: a propensity score matching study. Eur J Cardiothorac Surg. 2015;48(2):273–8.
Rivera C, Bernard A, Falcoz PE, et al. Characterization and prediction of prolonged air leak after pulmonary resection: a nationwide study setting up the index of prolonged air leak. Ann Thorac Surg. 2011;92(3):1062–8 (discussion 1068).
Altorki NK, Wang X, Wigle D, et al. Perioperative mortality and morbidity after sublobar versus lobar resection for early-stage non-small-cell lung cancer: post-hoc analysis of an international, randomised, phase 3 trial (calgb/alliance 140503). Lancet Respir Med. 2018;6(12):915–24.
Zhou B, Xu X, Dai J et al. Propensity-matched comparison of vats left upper tri-segmentectomy and lobectomy. Ann Thorac Surg. 2021. https://doi.org/10.1016/j.athoracsur.2021.07.057.
Handa Y, Tsutani Y, Mimae T, Miyata Y, Okada M. Complex segmentectomy in the treatment of stage IA non-small-cell lung cancer. Eur J Cardiothorac Surg. 2020;57(1):114–21.
Nomori H, Shiraishi A, Yamazaki I, et al. Extent of segmentectomy that achieves greater lung preservation than lobectomy. Ann Thorac Surg. 2021;112(4):1127–33.
Nakazawa S, Hanawa R, Nagashima T, Shimizu K, Yajima T, Shirabe K. Segmentectomy guided by 3-dimensional images reconstructed from nonenhanced computed tomographic data. Ann Thorac Surg. 2021;111(4):e301–4.
Acknowledgements
The authors are grateful to Yasuhiro Fukushima, Junya Fukuda, and Hiroyuki Takei, Department of Radiology, Gunma University Hospital, for obtaining 3D-CT images. We would like to thank Editage (http://ww.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ohtaki, Y., Yajima, T., Nagashima, T. et al. Complex vs. simple segmentectomy: comparing surgical outcomes in the left upper division. Gen Thorac Cardiovasc Surg 70, 962–970 (2022). https://doi.org/10.1007/s11748-022-01816-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-022-01816-4