Abstract
Objectives
An increasing number of patients visiting the dental office have a growing need for perioperative oral management (POM) to prevent postoperative complications. Therefore, it is necessary to determine which patients should receive preferential POM. This study investigated the dental status of patients scheduled to undergo surgery and addressed the priority for POM.
Methods
This retrospective study included a total of 150 patients who were scheduled to undergo surgery at the Department of Respiratory Surgery (DRS), Department of Neurological Surgery (DNS), Department of Gynecological Surgery (DGS), Department of Breast and Endocrine Surgery (DBES), and Department of Esophageal Surgery (DES) managed by the Perioperative Management Center of Okayama University Hospital. We compared the general and dental status of patients among the five groups.
Results
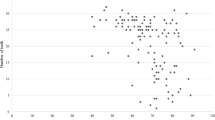
The DES group had significantly fewer teeth than the DBES group (p = 0.012), more severe periodontitis than both the DBES (p = 0.005) and DNS groups (p = 0.020), and poorer molar occlusal support status than both the DBES (p = 0.002) and DGS groups (p = 0.041). The DES group exhibited a significantly higher median age (p = 0.002), a higher ratio of males (p < 0.001), a higher prevalence of malignant tumors (p < 0.001), and higher proportions of smokers (p < 0.001) and drinkers (p < 0.001) than the other groups.
Conclusion
Patients who underwent surgery at the DES had more dental problems than other surgery patients. Accordingly, these patients should be given the highest priority for POM triage.



Similar content being viewed by others
References
Ding J, Sun B, Song P, Liu S, Chen H, Feng M, et al. The application of enhanced recovery after surgery (ERAS)/fast-track surgery in gastrectomy for gastric cancer: a systematic review and meta-analysis. Oncotarget. 2017;8:75699–711.
Takagi K, Yoshida R, Yagi T, Umeda Y, Nobuoka D, Kuise T, et al. Effect of an enhanced recovery after surgery protocol in patients undergoing pancreaticoduodenectomy: a randomized controlled trial. Clin Nutr. 2019;38:174–81.
Yasuhara T, Hishikawa T, Agari T, Kurozumi K, Ichikawa T, Kameda M, et al. Perioperative management center (PERIO) for neurosurgical patients. Neurol Med Chir (Tokyo). 2016;56:574–9.
Soutome S, Yanamoto S, Funahara M, Hasegawa T, Komori T, Yamada SI, et al. Effect of perioperative oral care on prevention of postoperative pneumonia associated with esophageal cancer surgery: a multicenter case–control study with propensity score matching analysis. Medicine (Baltimore). 2017;96:e7436.
Sato J, Goto J, Harahashi A, Murata T, Hata H, Yamazaki Y, et al. Oral health care reduces the risk of postoperative surgical site infection in inpatients with oral squamous cell carcinoma. Support Care Cancer. 2011;19:409–16.
Ishikawa S, Yamamori I, Takamori S, Kitabatake K, Edamatsu K, Sugano A, et al. Evaluation of effects of perioperative oral care intervention on hospitalization stay and postoperative infection in patients undergoing lung cancer intervention. Support Care Cancer. 2021;29:135–43.
Newland MC, Ellis SJ, Peters KR, Simonson JA, Durham TM, Ullrich FA, et al. Dental injury associated with anesthesia: a report of 161,687 anesthetics given over 14 years. J Clin Anesth. 2007;19:339–45.
Nawachi K, Soga K, Yamanaka R, Ashiwa T, Ito M, Sato M, et al. Necessity of measures for preventing intraoral complications during orotracheal intubation. J Jpn Soc Intensive Care Med. 2012;19:431–2.
Yamanaka-Kohno R, Shirakawa Y, Inoue-Minakuchi M, Yokoi A, Muro M, Kosaki H, et al. Association of dental occlusal support with the Prognostic Nutritional Index in patients with esophageal cancer who underwent esophagectomy. Esophagus. 2021;18:49–55.
World Health Organization. Oral health surveys: basic methods. 5th ed. Geneva: World Health Organization; 1997.
Eichner K. Renewed examination of group classification of partially edentulous arches by Eichner and application advices for studies on morbidity statistics. Stomatol DDR. 1990;40:321–5.
Kosaka T, Ono T, Yoshimuta Y, Kida M, Kikui M, Nokubi T, et al. The effect of periodontal status and occlusal support on masticatory performance: the Suita study. J Clin Periodontol. 2014;41:497–503.
Nishino T, Yoshida T, Inoue S, Aoyama M, Takizawa H, Tangoku A, et al. Perioperative oral management for esophageal cancer and lung cancer surgery. Nihon Geka Gakkai Zasshi. 2017;118:155–60.
Survey of Dental Diseases. Tokyo: Dental Health Division of Health Policy Bureau, Ministry of Health, Labour and Welfare Japan; 2011.
De Stefani E, Fierro L, Barrios E. Black (air-cured) and blond (flue-cured) tobacco and cancer risk. III: Oesophageal cancer. Eur J Cancer. 1993;29A:763–6.
Malhotra J, Malvezzi M, Negri E, La Vecchia C, Boffetta P. Risk factors for lung cancer worldwide. Eur Respir J. 2016;48:889–902.
Vaughan TL, Davis S, Kristal A, Thomas DB. Obesity, alcohol, and tobacco as risk factors for cancers of the esophagus and gastric cardia: adenocarcinoma versus squeamous cell carcinoma. Cancer Epidemiol Biomarkers Prev. 1995;4:85–92.
Reynolds MA. Modifiable risk factors in periodontitis: at the intersection of aging and disease. Periodontol. 2000;2014(64):7–19.
Moura-Grec PG, Marsicano JA, Carvalho CA, Sales-Peres SH. Obesity and periodontitis: systematic review and meta-analysis. Cien Saude Colet. 2014;19:1763–72.
Martinez-Herrera M, Silvestre-Rangil J, Silvestre FJ. Association between obesity and periodontal disease. A systematic review of epidemiological studies and controlled clinical trials. Med Oral Patol Oral Cir Bucal. 2017;22:e708–15.
Suvan J, D’Aiuto F, Moles DR, Petrie A, Donos N. Association between overweight/obesity and periodontitis in adults. A systematic review. Obes Rev. 2011;12:e381-404.
Wakabayashi H, Matsushima M, Ichikawa H, Murayama S, Yoshida S, Kaneko M, et al. Occlusal support, dysphagia, malnutrition, and activities of daily living in aged individuals needing long-term care: a path analysis. J Nutr Health Aging. 2018;22:53–8.
Tanaka T, Takahashi K, Hirano H, Kikutani T, Watanabe Y, Ohara Y, et al. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med. 2018;73:1661–7.
Yoshida N, Harada K, Baba Y, Kosumi K, Iwatsuki M, Kinoshita K, et al. Preoperative controlling nutritional status (CONUT) is useful to estimate the prognosis after esophagectomy for esophageal cancer. Langenbecks Arch Surg. 2017;402:333–41.
Donington JS. Functional conduit disorders after esophagectomy. Thorac Surg Clin. 2006;16:53–62.
Yamanaka R, Soga Y, Minakuchi M, Nawachi K, Maruyama T, Kuboki T, et al. Occlusion and weight change in a patient after esophagectomy: success derived from restoration of occlusal support. Int J Prosthodont. 2013;26:574–6.
Wakabayashi H, Uwano R. Rehabilitation nutrition for possible sarcopenic dysphagia after lung cancer surgery: a case report. Am J Phys Med Rehabil. 2016;95:e84–9.
Kaneoka A, Yang S, Inokuchi H, Ueha R, Yamashita H, Nito T, et al. Presentation of oropharyngeal dysphagia and rehabilitative intervention following esophagectomy: a systematic review. Dis Esophagus. 2018;31:doy050.
Keeling WB, Lewis V, Blazick E, Maxey TS, Garrett JR, Sommers KE, et al. Routine evaluation for aspiration after thoracotomy for pulmonary resection. Ann Thorac Surg. 2007;83:193–6.
Iwata E, Hasegawa T, Yamada SI, Kawashita Y, Yoshimatsu M, Mizutani T, et al. Effects of perioperative oral care on prevention of postoperative pneumonia after lung resection: multicenter retrospective study with propensity score matching analysis. Surgery. 2019;165:1003–7.
Talwar JS, Gaiser RR. Dental injury during general anesthesia and those who seek financial compensation: a retrospective study. J Clin Anesth. 2020;63:109757.
Sato Y, Motoyama S, Takano H, Nakata A, Liu J, Harimaya D, et al. Esophageal cancer patients have a high incidence of severe periodontitis and preoperative dental care reduces the likelihood of severe pneumonia after esophagectomy. Dig Surg. 2016;33:495–502.
Acknowledgements
The authors are deeply grateful to the team members at the PERiO, Okayama University Hospital. This work was supported by the Japan Society for the Promotion of Science (JSPS) and the Ministry of Education, Culture, Sports, Science, and Technology (MEXT) through a Grant-in-Aid for Scientific Research (KAKENHI) (C) (Nos. 19K10444, C16K11857, and 16K11858) and a Grant-in-Aid for Young Scientists (B) (No. 25862082).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamanaka-Kohno, R., Shirakawa, Y., Yokoi, A. et al. Patients scheduled to undergo esophageal surgery should have the highest priority for perioperative oral management triage: a cross-sectional study. Gen Thorac Cardiovasc Surg 70, 378–385 (2022). https://doi.org/10.1007/s11748-021-01757-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01757-4