Abstract
Objective
The induction of artificial pneumothorax has many intraoperative advantages. However, few reports on the postoperative effects of artificial pneumothorax induction are available. In this study, we investigated the effect of artificial pneumothorax on postoperative clinical course in patients with mediastinal tumors.
Methods
We retrospectively investigated the clinical courses of 89 patients who had undergone mediastinal tumor resection between January 2010 and December 2020. Sixty-five patients had undergone resection with artificial pneumothorax.
Results
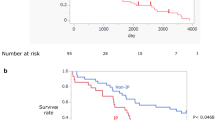
The tumor location significantly varied across patients. The proportion of patients in whom artificial pneumothorax was induced was higher among those having anterior mediastinal tumors. The number of ports and the total skin incision length were significantly higher in patients without artificial pneumothorax. The C-reactive protein level elevation on postoperative day 2 and pleural effusion at 24 h after surgery were significantly higher in patients without artificial pneumothorax. Furthermore, the albumin level reduction and hospital stay after surgery were significantly lower in patients with artificial pneumothorax. Multiple regression analysis showed that the use of artificial pneumothorax was an independent predictive factor of the C-reactive protein level elevation on postoperative day 2 and pleural effusion at 24 h after surgery. In patients without artificial pneumothorax, the operation time positively correlated with the C-reactive protein level (r = 0.646, P < 0.001).
Conclusions
Artificial pneumothorax suppressed the postoperative inflammatory response, pleural effusion, and albumin reduction, and shortened the hospital stay in patients undergoing mediastinal tumor surgery.



Similar content being viewed by others
References
Nomura S, Tsujimoto H, Ishibashi Y, Fujishima S, Kouzu K, Harada M, et al. Efficacy of artificial pneumothorax under two-lung ventilation in video-assisted thoracoscopic surgery for esophageal cancer. Surgical Endosc. 2020;34:5501–7.
Palanivelu C, Prakash A, Senthilkumar R, Senthilnathan P, Parthasarathi R, Rajan PS, et al. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position–experience of 130 patients. J Am Coll Surg. 2006;203:7–16.
Zhao M, Jiang T, Li M, Yang X, Dai X, Shen Y, et al. Video-assisted thoracoscopic total thymectomy: two-lung ventilation with artificial pneumothorax. Minim Invasive Ther Allied Technol. 2020;29:380–4.
Takemura M, Kaibe N, Takii M, Sasako M. Operative benefits of artificial pneumothorax in thoracoscopic esophagectomy in the left lateral decubitus position for esophageal cancer. Int J Clin Med. 2015;06:8.
Hanly EJ, Mendoza-Sagaon M, Murata K, Hardacre JM, De Maio A, Talamini MA. CO2 Pneumoperitoneum modifies the inflammatory response to sepsis. Ann Surg. 2003;237:343–50.
Jatzko GR, Lisborg PH, Pertl AM, Stettner HM. Multivariate comparison of complications after laparoscopic cholecystectomy and open cholecystectomy. Ann Surg. 1995;221:381–6.
Vittimberga FJ Jr, Foley DP, Meyers WC, Callery MP. Laparoscopic surgery and the systemic immune response. Ann Surg. 1998;227:326–34.
Watson RW, Redmond HP, McCarthy J, Burke PE, Bouchier-Hayes D. Exposure of the peritoneal cavity to air regulates early inflammatory responses to surgery in a murine model. Br J Surg. 1995;82:1060–5.
Tsukioka T, Takemura S, Minamiyama Y, Nishiyama N, Mizuguchi S, Okada S, et al. Local and systemic impacts of pleural oxygen exposure in thoracotomy. BioFactors. 2007;30:117–28.
Sancheti MS, Dewan BP, Pickens A, Fernandez FG, Miller DL, Force SD. Thoracoscopy without lung isolation utilizing single lumen endotracheal tube intubation and carbon dioxide insufflation. Ann Cardiothorac Surg. 2013;96:439–44.
Suda T, Ashikari S, Tochii S, Sugimura H, Hattori Y. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Cardiothorac Surg. 2014;97:718–9.
Neumaier M, Scherer MA. C-reactive protein levels for early detection of postoperative infection after fracture surgery in 787 patients. Acta Orthop. 2008;79:428–32.
Swanson SJ, Herndon JE 2nd, D’Amico TA, Demmy TL, McKenna RJ Jr, Green MR, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802—a prospective, multi-institution feasibility study. J Clin Oncol. 2007;25:4993–7.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Guyton AC, Hall JE. Transport of oxygen and carbon dioxide in the blood and body fluids. In: Guyton AC, Hall JE, editors. Textbook of medical physiology. 10th ed. Philadelphia: W.B. Saunders; 2000. p. 464–73.
Light RW, Macgregor MI, Luchsinger PC, Ball WC Jr. Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med. 1972;77:507–13.
Lim S, Koh A. Nutrition and the elderly surgical patients. MOJ Surg. 2017;4:114–20.
Ye B, Tantai JC, Li W, Ge XX, Feng J, Cheng M, et al. Video-assisted thoracoscopic surgery versus robotic-assisted thoracoscopic surgery in the surgical treatment of Masaoka stage I thymoma. World J Surg Oncol. 2013;11:157.
Şehitogullari A, Nasır A, Anbar R, Erdem K, Bilgin C. Comparison of perioperative outcomes of videothoracoscopy and robotic surgical techniques in thymoma. Asian J Surg. 2020;43:244–50.
Haruki T, Kubouchi Y, Takagi Y, Kidokoro Y, Matsui S, Nakanishi A, et al. Comparison of medium-term survival outcomes between robot-assisted thoracoscopic surgery and video-assisted thoracoscopic surgery in treating primary lung cancer. Gen Thorac Cardiovasc Surg. 2020;68:984–92.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
The local institutional ethics committee approved this study (approval no. 2020-247; approval date, January 7, 2021).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ito, R., Tsukioka, T., Izumi, N. et al. Artificial pneumothorax suppresses postoperative inflammatory reaction in mediastinal tumor surgery. Gen Thorac Cardiovasc Surg 70, 257–264 (2022). https://doi.org/10.1007/s11748-021-01716-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01716-z