Abstract
Objective
To evaluate the effects of administering tranexamic acid (TXA) after cardiopulmonary bypass, instead of after anesthesia induction, on postoperative seizures and blood transfusion requirements.
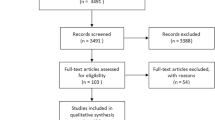
Methods
Adult patients who underwent valve surgery and/or coronary artery bypass grafting at West China Hospital between July 1, 2011 and December 31, 2016 were retrospectively analyzed. Patients either received TXA after bypass (n = 2062) or not (n = 4236). Logistic regression and propensity score matching analysis were performed to assess effects of TXA on postoperative seizures and blood product requirements in hospital.
Results
Among 6298 patients, seizures occurred in 2.4% (102/4236) in the no-TXA group and 2.7% (56/2062) in the TXA group (P = 0.46). The number of patients receiving any blood products was greater in the no-TXA group (57.3%, 2428/4236) than in the TXA group (53.1%, 1095/2062) (P < 0.01), and the volume of blood products was also greater in the no-TXA group (1.5 vs. 1.0 units, P < 0.01). TXA was not associated with increased incidence of postoperative seizures (adjusted OR 1.16, 95% CI 0.83–1.62) but was associated with lower incidence of a requirement for blood products (adjusted OR 0.82, 95% CI 0.73–0.92). Similar results were obtained after patients from the two groups were matched based on propensity scoring. TXA was associated with reduced requirements for fresh frozen plasma, platelets and cryoprecipitate, but not red blood cells.
Conclusions
Administering TXA after bypass may reduce requirements for blood products without increasing risk of seizures following cardiac surgery.


Similar content being viewed by others
References
Paparella D, Guida P, Scrascia G, Fanelli V, Contini M, Zaccaria S, et al. On-pump versus off-pump coronary artery bypass surgery in patients with preoperative anemia. J Thorac Cardiovasc Surg. 2015;149(4):1018–26.
Casati V, Gerli C, Franco A, Della Valle P, Benussi S, Alfieri O, et al. Activation of coagulation and fibrinolysis during coronary surgery: on-pump versus off-pump techniques. Anesthesiology. 2001;95(5):1103–9.
Dixon B, Santamaria J, Campbell D. Coagulation activation and organ dysfunction following cardiac surgery. Chest. 2005;128(1):229–36.
Menkis AH, Martin J, Cheng DC, Fitzgerald DC, Freedman JJ, Gao C, et al. Drug, devices, technologies, and techniques for blood management in minimally invasive and conventional cardiothoracic surgery: a consensus statement from the International Society for Minimally Invasive Cardiothoracic Surgery (ISMICS) 2011. Innovations (Phila). 2012;7(4):229–41.
Horrow JC, Van Riper DF, Strong MD, Brodsky I, Parmet JL. Hemostatic effects of tranexamic acid and desmopressin during cardiac surgery. Circulation. 1991;84(5):2063–70.
Nuttall GA, Oliver WC, Ereth MH, Santrach PJ, Bryant SC, Orszulak TA, et al. Comparison of blood-conservation strategies in cardiac surgery patients at high risk for bleeding. Anesthesiology. 2000;92(3):674–82.
Murkin JM, Falter F, Granton J, Young B, Burt C, Chu M. High-dose tranexamic acid is associated with nonischemic clinical seizures in cardiac surgical patients. Anesth Analg. 2010;110(2):350–3.
Myles PS, Smith JA, Forbes A, Silbert B, Jayarajah M, Painter T, et al. Tranexamic acid in patients undergoing coronary-artery surgery. N Engl J Med. 2017;376(2):136–48.
Goldstone AB, Bronster DJ, Anyanwu AC, Goldstein MA, Filsoufi F, Adams DH, et al. Predictors and outcomes of seizures after cardiac surgery: a multivariable analysis of 2,578 patients. Ann Thorac Surg. 2011;91(2):514–8.
Sharma V, Katznelson R, Jerath A, Garrido-Olivares L, Carroll J, Rao V, et al. The association between tranexamic acid and convulsive seizures after cardiac surgery: a multivariate analysis in 11 529 patients. Anaesthesia. 2014;69(2):124–30.
Fergusson DA, Hebert PC, Mazer CD, Fremes S, MacAdams C, Murkin JM, et al. A comparison of aprotinin and lysine analogues in high-risk cardiac surgery. N Engl J Med. 2008;358(22):2319–31.
Gertler R, Gruber M, Grassin-Delyle S, Urien S, Martin K, Tassani-Prell P, et al. Pharmacokinetics of tranexamic acid in neonates and infants undergoing cardiac surgery. Br J Clin Pharmacol. 2017;83(8):1745–57.
Koster A, Borgermann J, Zittermann A, Lueth JU, Gillis-Januszewski T, Schirmer U. Moderate dosage of tranexamic acid during cardiac surgery with cardiopulmonary bypass and convulsive seizures: incidence and clinical outcome. Br J Anaesth. 2013;110(1):34–40.
Edmunds LH. Cardiopulmonary bypass after 50 years. N Engl J Med. 2004;351(16):1603–6.
Zhou ZF, Zhang FJ, Huo YF, Yu YX, Yu LN, Sun K, et al. Intraoperative tranexamic acid is associated with postoperative stroke in patients undergoing cardiac surgery. PLoS ONE. 2017;12(5):e0177011.
Boyle EMJ, Verrier ED, Spiess BD. Endothelial cell injury in cardiovascular surgery: the procoagulant response. Ann Thorac Surg. 1996;62(5):1549–57.
Qiu Y, Lin J, Yang Y, Zhou J, Gong LN, Qin Z, et al. Lack of efficacy of ulinastatin therapy during cardiopulmonary bypass surgery. Chin Med J (Engl). 2015;128(23):3138–42.
Lin J, Tan Z, Yao H, Hu X, Zhang D, Zhao Y, et al. Retrograde Inferior Vena caval Perfusion for Total Aortic arch Replacement Surgery (RIVP-TARS): study protocol for a multicenter, randomized controlled trial. Trials. 2019;20(1):232.
Fisher RS, van Emde BW, Blume W, Elger C, Genton P, Lee P, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(4):470–2.
Guo Y, Tang J, Du L, Liu J, Liu RC, Liu X, et al. Protamine dosage based on two titrations reduces blood loss after valve replacement surgery: a prospective, double-blinded, randomized study. Can J Cardiol. 2012;28(5):547–52.
Liu J, Chen CW, Huang D, Luo D, Du L. Effects of tranexamic acid after cardiopulmonary bypass on the outcomes of patients undergoing cardiac surgery. Sichuan Da Xue Xue Bao Yi Xue Ban. 2018;49(4):660–4.
Sander M, Spies CD, Martiny V, Rosenthal C, Wernecke KD, von Heymann C. Mortality associated with administration of high-dose tranexamic acid and aprotinin in primary open-heart procedures: a retrospective analysis. Crit Care. 2010;14(4):R148.
Keyl C, Uhl R, Beyersdorf F, Stampf S, Lehane C, Wiesenack C, et al. High-dose tranexamic acid is related to increased risk of generalized seizures after aortic valve replacement. Eur J Cardiothorac Surg. 2011;39(5):e114–21.
Hunter GR, Young GB. Seizures after cardiac surgery. J Cardiothorac Vasc Anesth. 2011;25(2):299–305.
Manji RA, Grocott HP, Leake J, Ariano RE, Manji JS, Menkis AH, et al. Seizures following cardiac surgery: the impact of tranexamic acid and other risk factors. Can J Anaesth. 2012;59(1):6–13.
Martin K, Knorr J, Breuer T, Gertler R, Macguill M, Lange R, et al. Seizures after open heart surgery: comparison of epsilon-aminocaproic acid and tranexamic acid. J Cardiothorac Vasc Anesth. 2011;25(1):20–5.
Martin K, Wiesner G, Breuer T, Lange R, Tassani P. The risks of aprotinin and tranexamic acid in cardiac surgery: a one-year follow-up of 1188 consecutive patients. Anesth Analg. 2008;107(6):1783–90.
Berman M, Cardone D, Sharples L, Vuylsteke A, Klein A, Gerrard C, et al. Safety and efficacy of aprotinin and tranexamic acid in pulmonary endarterectomy surgery with hypothermia: review of 200 patients. Ann Thorac Surg. 2010;90(5):1432–6.
Gofton TE, Chu MW, Norton L, Fox SA, Chase L, Murkin JM, et al. A prospective observational study of seizures after cardiac surgery using continuous EEG monitoring. Neurocrit Care. 2014;21(2):220–7.
Montes FR, Pardo DF, Carreno M, Arciniegas C, Dennis RJ, Umana JP. Risk factors associated with postoperative seizures in patients undergoing cardiac surgery who received tranexamic acid: a case-control study. Ann Card Anaesth. 2012;15(1):6–12.
Manji RA, Grocott HP, Manji JS, Menkis AH, Jacobsohn E. Recurrent seizures following cardiac surgery: risk factors and outcomes in a historical cohort study. J Cardiothorac Vasc Anesth. 2015;29(5):1206–11.
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med. 1996;335(25):1857–63.
Furtmuller R, Schlag MG, Berger M, Hopf R, Huck S, Sieghart W, et al. Tranexamic acid, a widely used antifibrinolytic agent, causes convulsions by a gamma-aminobutyric acid(A) receptor antagonistic effect. J Pharmacol Exp Ther. 2002;301(1):168–73.
Kratzer S, Irl H, Mattusch C, Burge M, Kurz J, Kochs E, et al. Tranexamic acid impairs gamma-aminobutyric acid receptor type A-mediated synaptic transmission in the murine amygdala: a potential mechanism for drug-induced seizures? Anesthesiology. 2014;120(3):639–49.
Casati V, Bellotti F, Gerli C, Franco A, Oppizzi M, Cossolini M, et al. Tranexamic acid administration after cardiac surgery: a prospective, randomized, double-blind, placebo-controlled study. Anesthesiology. 2001;94(1):8–14.
Spence J, Long S, Tidy A, Raymer K, Devereaux PJ, Lamy A, et al. Tranexamic acid administration during on-pump cardiac surgery: a survey of current practices among Canadian anesthetists working in academic centers. Anesth Analg. 2017.
Acknowledgements
The authors would like to thank Professor Jerry Yu, M.D., Ph.D. in the Department of Pulmonary Medicine at the University of Louisville School of Medicine for advice and revision of the manuscript, and Dr. Linyu Tian in the Department of Neurology, West China Hospital, Sichuan University for the diagnosis of postoperative seizures.
Funding
This work was supported by the 1.3.5 Project for Disciplines of Excellence, West China Hospital of Sichuan University (20HXJS004 to LD).
Author information
Authors and Affiliations
Contributions
Conceptualization: LD, JL. Data curation: CC, JL. Formal analysis: CC, JL. Funding acquisition: LD. Investigation: CC, JL. Methodology: CC, JL, LD. Project administration: CC, JL. Supervision: CC, JL, LD. Writing—original draft: CC, JL. Writing—review and editing: LD, CC.
Corresponding author
Ethics declarations
Conflict of interest
Jing Liu has no conflict of interest. Changwei Chen has no conflict of interest. Lei Du has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, C., Liu, J. & Du, L. Tranexamic acid after cardiopulmonary bypass does not increase risk of postoperative seizures: a retrospective study. Gen Thorac Cardiovasc Surg 70, 337–346 (2022). https://doi.org/10.1007/s11748-021-01709-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01709-y