Abstract
Objective
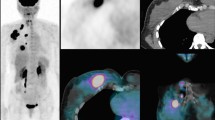
The surgical result of early-staged lung cancer is not satisfactory due to unexpected postoperative lymph node metastasis and recurrence. This study aimed to investigate which preoperative factors—including the standard uptake value max (SUVmax) of positron emission tomography—could predict occult lymph node metastasis and survival.
Methods
We retrospectively analyzed data from 598 patients with clinical stage I lung cancer who underwent surgery, and examined their preoperative clinical characteristics.
Results
A total of 1586 patients had surgery for primary lung cancer between 2006 and 2019; 598 patients with clinical stage I lung cancer were the study inclusion; occult lymph node metastasis was detected in 102 (17.1%). Univariable and multivariable analyses showed that SUVmax ≥ 3 (P < 0.001), clinical invasive tumor size ≥ 2 cm (P = 0.009), and carcinoembryonic antigen > 5 (P = 0.03) were associated with significant risk factors rated (%) for occult lymph node metastasis, as follows: high-risk group (three factors), moderate-risk group (two factors) and low-risk group (one factor or none) corresponding to 32.2 (28/87), 22.8 (41/180) and 7.3 (19/262), respectively (P < 0.001). The 5-year overall survival rates (%) of patients without lymph node metastasis holding SUVmax 6 or over were as poor as those of patients with lymph node metastasis (72.0% vs 64.1%; P = 0.56).
Conclusions
We might consider wedge resection or segmentectomy, omitting lymphadenectomy, for the low-risk group; adjuvant therapy is indicated for patients without lymph node metastasis having SUVmax 6 or over.



Similar content being viewed by others
References
Minn H, Zasadny KR, Quint LE, Wahl RL. Lung cancer: reproducibility of quantitative measurements for evaluating 2-[F-18]-fluoro-2-deoxy-d-glucose uptake at PET. Radiology. 1995;196:167–73.
Bollineni VR, Ytre-Hauge S, Bollineni-Balabay O, Salvesen HB, Haldorsen IS. High diagnostic value of 18F-FDG PET/CT in endometrial cancer: systematic review and meta-analysis of the literature. J Nucl Med. 2016;57:879–85.
Goel R, Moore W, Sumer B, Khan S, Sher D, Subramaniam RM. clinical practice in PET/CT for the management of head and neck squamous cell cancer. AJR Am J Roentgenol. 2017;209:289–303.
Fischer B, Lassen U, Mortensen J, Larsen S, Loft A, Bertelsen A, et al. Preoperative staging of lung cancer with combined PET-CT. N Engl J Med. 2009;361:32–9.
Zhao L, He ZY, Zhong XN, Cui ML. (18)FDG-PET/CT for detection of mediastinal nodal metastasis in non-small cell lung cancer: a meta-analysis. Surg Oncol. 2012;21:230–6.
Takahashi Y, Suzuki S, Matsutani N, Kawamura M. 18F-fluorodeoxyglucose positron emission tomography/computed tomography in the evaluation of clinically node-negative non-small cell lung cancer. Thorac Cancer. 2019;10:413–20.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Rami-Porta R, Bolejack V, Giroux DJ, Chansky K, Crowley J, Asamura H, et al. The IASLC lung cancer staging project: the new database to inform the eighth edition of the TNM classification of lung cancer. J Thorac Oncol. 2014;9:1618–24.
Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC. Pathology and genetics of tumours of the lung, pleura, thymus and heart. In: Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC, editors. World Health Organization classification of tumours. Lyon: IARC Press; 2004. p. 9–124.
Cerfolio RJ, Bryant AS, Ohja B, Bartolucci AA. The maximum standardized uptake values on positron emission tomography of a non-small cell lung cancer predict stage, recurrence, and survival. J Thorac Cardiovasc Surg. 2005;130:151–9.
Okada M, Nakayama H, Okumura S, Daisaki H, Adachi S, Yoshimura M, et al. Multicenter analysis of high-resolution computed tomography and positron emission tomography/computed tomography findings to choose therapeutic strategies for clinical stage IA lung adenocarcinoma. J Thorac Cardiovasc Surg. 2011;141:1384–91.
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, et al. Solid tumor size on high-resolution computed tomography and maximum standardized uptake on positron emission tomography for new clinical T descriptors with T1 lung adenocarcinoma. Ann Oncol. 2013;24:2376–81.
Hung JJ, Yeh YC, Jeng WJ, Wu YC, Chou TY, Hsu WH. Factors predicting occult lymph node metastasis in completely resected lung adenocarcinoma of 3 cm or smaller. Eur J Cardiothorac Surg. 2016;50:329–36.
Moon Y, Kim KS, Lee KY, Sung SW, Kim YK, Park JK. Clinicopathologic factors associated with occult lymph node metastasis in patients with clinically diagnosed N0 lung adenocarcinoma. Ann Thorac Surg. 2016;101:1928–35.
Seto K, Kuroda H, Yoshida T, Sakata S, Mizuno T, Sakakura N, et al. Higher frequency of occult lymph node metastasis in clinical N0 pulmonary adenocarcinoma with ALK rearrangement. Cancer Manag Res. 2018;10:2117–24.
Decaluwé H, Moons J, Fieuws S, De Wever W, Deroose C, Stanzi A, et al. Is central lung tumour location really predictive for occult mediastinal nodal disease in (suspected) non-small-cell lung cancer staged cN0 on 18F-fluorodeoxyglucose positron emission tomography-computed tomography? Eur J Cardiothorac Surg. 2018;54:134–40.
Zhang C, Pang G, Ma C, Wu J, Wang P, Wang K. Preoperative risk assessment of lymph node metastasis in cT1 lung cancer: a retrospective study from Eastern China. J Immunol Res. 2019;2019:6263249.
Moon Y, Choi SY, Park JK, Lee KY. Risk Factors for occult lymph node metastasis in peripheral non-small cell lung cancer with invasive component size 3 cm or less. World J Surg. 2020;44:1658–65.
Vaghjiani RG, Takahashi Y, Eguchi T, Lu S, Kameda K, Tano Z, et al. Tumor spread through air spaces is a predictor of occult lymph node metastasis in clinical stage IA lung adenocarcinoma. J Thorac Oncol. 2020;15:792–802.
Yasufuku K, Pierre A, Darling G, de Perrot M, Waddell T, Johnston M, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg. 2011;142:1393-400.e1.
De Leyn P, Dooms C, Kuzdzal J, Lardinois D, Passlick B, Rami-Porta R, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2014;45:787–98.
Silvestri GA, Gonzalez AV, Jantz MA, Margolis ML, Gould MK, Tanoue LT, et al. Methods for staging non-small cell lung cancer: diagnosis and management of lung cancer, 3rd Ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2013;143(5 Suppl):e211S-e250S.
Grutters JP, Kessels AG, Pijls-Johannesma M, De Ruysscher D, Joore MA, Lambin P. Comparison of the effectiveness of radiotherapy with photons, protons and carbon-ions for non-small cell lung cancer: a meta-analysis. Radiother Oncol. 2010;95:32–40.
Bedetti B, Bertolaccini L, Rocco R, Schmidt J, Solli P, Scarci M. Segmentectomy versus lobectomy for stage I non-small cell lung cancer: a systematic review and meta-analysis. J Thorac Dis. 2017;9:1615–23.
Wang D, Zhang M, Gao X, Yu L. Prognostic value of baseline 18F-FDG PET/CT functional parameters in patients with advanced lung adenocarcinoma stratified by EGFR mutation status. PLoS ONE. 2016;11:e0158307.
Acknowledgments
We are very grateful to Enago for English proofreading.
Funding
This study received no funding from any institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hino, H., Utsumi, T., Maru, N. et al. Clinical impact and utility of positron emission tomography on occult lymph node metastasis and survival: radical surgery for stage I lung cancer. Gen Thorac Cardiovasc Surg 69, 1196–1203 (2021). https://doi.org/10.1007/s11748-021-01606-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01606-4