Abstract
Objective
This study aimed to evaluate the recurrence rate after primary and secondary conservative treatments and to clarify the validity of current primary spontaneous pneumothorax management by comparing secondary conservative treatment and surgical outcomes.
Methods
Data from 166 patients with primary spontaneous pneumothorax treated at a single site between September 2015 and March 2019 were retrospectively evaluated. Patient characteristics of those who received primary conservative therapy (n = 166) and secondary conservative therapy (n = 28) were summarized. The outcomes from patients who experienced recurrence (n = 64) were compared based on those who underwent surgery (n = 24) and those who underwent secondary conservative therapy (n = 28).
Results
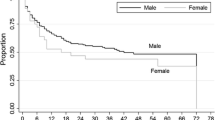
The post-treatment day 60 recurrence rate was 27.1 and 49.5% cases in the primary and secondary treatment groups, respectively, which was significantly higher after secondary treatment than after primary treatment with conservative therapy (p = 0.032). The post-treatment one-year recurrence rate was 13.5 and 57.9% in patients who underwent surgery and secondary conservative treatment, respectively; secondary conservative treatment resulted in a significantly higher recurrence rate than surgery (p < 0.001).
Conclusions
There is evidence for guidelines that recommend surgery for recurrent primary spontaneous pneumothorax after primary conservative therapy based on its lower and more delayed post-treatment recurrence rate than secondary treatment with conservative therapy.



Similar content being viewed by others
References
Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001;119:590–602.
MacDuff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline. Thorax. 2010;65(Suppl 2):ii18-31.
Tschopp JM, Bintcliffe O, Astoul P, Canalis E, Driesen P, Janssen J, et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J. 2015;46:321–35.
Chen JS, Chan WK, Tsai KT, Hsu HH, Lin CY, Yuan A, et al. Simple aspiration and drainage and intrapleural minocycline pleurodesis versus simple aspiration and drainage for the initial treatment of primary spontaneous pneumothorax: an open-label, parallel-group, prospective, randomized, controlled trial. Lancet. 2013;381:1277–82.
Sadikot RT, Greene T, Meadows K, Arnold AG. Recurrence of primary spontaneous pneumothorax. Thorax. 1997;52:805–9.
Park S, Jang HJ, Song JH, Bae SY, Kim H, Nam SH, et al. Do blebs or bullae on high-resolution computed tomography predict ipsilateral recurrence in young patients at the first episode of primary spontaneous pneumothorax? Korean J Thorac Cardiovasc Surg. 2019;52:91–9.
Chambers A, Scarci M. In patients with first-episode primary spontaneous pneumothorax is video-assisted thoracoscopic surgery superior to tube thoracostomy alone in terms of time to resolution of pneumothorax and incidence of recurrence? Interact Cardiovasc Thorac Surg. 2009;9:1003–8.
Huang H, Ji H, Tian H. Risk factors for recurrence of primary spontaneous pneumothorax after thoracoscopic surgery. Biosci Trends. 2015;9:193–7.
Noh D, Lee S, Haam SJ, Paik HC, Lee DY. Recurrence of primary spontaneous pneumothorax in young adults and children. Interact Cardiovasc Thorac Surg. 2015;21:195–9.
Nakayama T, Takahashi Y, Uehara H, Matsutani N, Kawamura M. Outcome and risk factors of recurrence after thoracoscopic bullectomy in young adults with primary spontaneous pneumothorax. Surg Today. 2017;47:859–64.
Schramel FM, Sutedja TG, Braber JC, van Mourik JC, Postmus PE. Cost-effectiveness of video-assisted thoracoscopic surgery versus conservative treatment for first time or recurrent spontaneous pneumothorax. Eur Respir J. 1996;9:1821–5.
Sawada S, Watanabe Y, Moriyama S. Video-assisted thoracoscopic surgery for primary spontaneous pneumothorax: evaluation of indications and long-term outcome compared with conservative treatment and open thoracotomy. Chest. 2005;127:2226–30.
Tsuboshima K, Matoba Y, Wakahara T, Maniwa Y. Natural history of bulla neogenesis for primary spontaneous pneumothorax: a propensity score analysis. Gen Thorac Cardiovasc Surg. 2019;67:464–9.
Kim D, Shin HJ, Kim SW, Hong JM, Lee KS, Lee SH. Psychological problems of pneumothorax according to resilience, stress, and post-traumatic stress. Psychiatry Investig. 2017;14:795–800.
Lee SH, Choi H, Kim S, Choi TK, Lee S, Kim B, et al. Association between anger and first-onset primary spontaneous pneumothorax. Gen Hosp Psychiatry. 2008;30:331–6.
Noppen M, Alexander P, Driesen P, Slabbynck H, Verstraeten A. Manual aspiration versus chest tube drainage in first episodes of primary spontaneous pneumothorax: a multicenter, prospective, randomized pilot study. Am J Respir Crit Care Med. 2002;165:1240–4.
Chen J, Volpi S, Ali JM, Aresu G, Wu L, Chen Z, et al. Comparison of post-operative pain and quality of life between uniportal subxiphoid and intercostal video-assisted thoracoscopic lobectomy. J Thorac Dis. 2020;12:3582–90.
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsuboshima, K., Kurihara, M., Nonaka, Y. et al. Is conventional management of primary spontaneous pneumothorax appropriate?. Gen Thorac Cardiovasc Surg 69, 716–721 (2021). https://doi.org/10.1007/s11748-020-01535-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-020-01535-8