Abstract
Objective
In minimally invasive cardiac surgery (MICS), femoral artery cannulation during cardiopulmonary bypass (CPB) can cause limb ischemia. This study evaluated the association between femoral artery anatomy and the risk of limb ischemia in MICS.
Methods
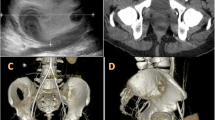
Eighty-one patients who underwent MICS with CPB using single femoral artery cannulation between 2010 and 2018 were included. The patients were stratified by their femoral artery diameter and anatomy of ectopic side branch, i.e., medial or lateral femoral circumflex arteries: Type A, deep femoral artery (DFA) ≥ superficial femoral artery (SFA); type B, DFA < SFA with an ectopic side branch of the common femoral artery (CFA); type C, DFA < SFA with an ectopic side branch at the CFA bifurcation; and type D, DFA < SFA without an ectopic side branch. The ratio of the postoperative creatine kinase concentration and the cross-sectional area of the femoral muscles (CK/MA) was used as a surrogate marker of limb ischemia. Predictors of high CK/MA were evaluated.
Results
No critical limb ischemia was observed in this study. The median postoperative creatine kinase and CK/MA were 1954 (1305–2872) IU/l and 15.2 (9.2–19.8) IU/l/cm2. Multivariable logistic regression found that anatomical type D (odds ratio 4.19, 95% confidence interval: (1.26–14.0); p = 0.020) and prolonged CPB time (OR 1.01, 95% CI (1.00–1.02); p = 0.045) were independent risk factors of high CK/MA.
Conclusion
Anatomical type D and prolonged CPB time were associated with risk of limb ischemia in MICS.


Similar content being viewed by others
References
Wadhawa VA, Patel KG, Doshi CP, Shah JK, Ramani JA, Garg PD, et al. Direct femoral cannulation in minimal invasive pediatric cardiac surgery: our experience with midterm result. Innovations. 2018;13:300–4.
Pozzi M, Henaine R, Grinberg D, Robin J, Saroul C, Delannoy B, et al. Total percutaneous femoral vessels cannulation for minimally invasive mitral valve surgery. Ann Cardiothorac Surg. 2013;2:739–43.
Lamelas J, Williams RF, Mawad M, LaPietra A. Complications associated with femoral cannulation during minimally invasive cardiac surgery. Ann Thorac Surg. 2017;103:1927–32.
Saadat S, Schultheis M, Azzolini A, Romero J, Dombrovskiy V, Odroniec K, et al. Femoral cannulation: a safe vascular access option for cardiopulmonary bypass in minimally invasive cardiac surgery. Perfusion. 2016;31:131–4.
Vander Salm TJ. Prevention of lower extremity ischemia during cardiopulmonary bypass via femoral cannulation. Ann Thorac Surg. 1997;63:251–2.
Vida VL, Padalino MA, Boccuzzo G, Stellin G. Near-infrared spectroscopy for monitoring leg perfusion during minimally invasive surgery for patients with congenital heart defects. J Thorac Cardiovasc Surg. 2012;143:756–7.
Bonaros N, Wiedemann D, Nagiller J, Feuchtner G, Kolbitsch C, Kaufmann M, et al. Distal leg protection for peripheral cannulation in minimally invasive and totally endoscopic cardiac surgery. Heart Surg Forum. 2009;12:E158–62.
Tarui T, Miyata K, Shigematsu S, Watanabe G. Risk factors to predict leg ischemia in patients undergoing single femoral artery cannulation in minimally invasive cardiac surgery. Perfusion. 2018;33:533–7.
Toya T, Fujita T, Fukushima S, Shimahara Y, Kume Y, Yamashita K, et al. Efficacy of regional saturation of oxygen monitor using near-infrared spectroscopy for lower limb ischemia during minimally invasive cardiac surgery. J Artif Organs. 2018;21:420–6.
Tsiouris A, Elkinany S, Ziganshin BA, Elefteriades JA. Open Seldinger-guided femoral artery cannulation technique for thoracic aortic surgery. Ann Thorac Surg. 2016;101:2231–5.
Monghadam-Kia S, Oddis CV, Aggarwal R. Approach to asymptomatic creatine kinase elevation. Cleve Clin J Med. 2016;83:37–42.
Kim TN, Park MS, Lee EJ, Chung HS, Yoo HJ, Kang HJ, et al. Comparisons of three different methods for defining sarcopenia: an aspect of cardiometabolic risk. Sci Rep. 2017;7:6491. https://doi.org/10.1038/s41598-017-06831-7.
Atluri P, Goldstone AB, Fox J, Szeto WY, Hargrove WC. Port access cardiac operations can be safely performed with either endoaortic balloon or Chitwood clamp. Ann Thorac Surg. 2014;98:1579–83.
Bongert M, Gehron J, Geller M, Böning A, Grieshaber P. Cannula position and Bernoulli effect contribute to leg malperfusion during extracorporeal life support with femoral arterial cannulation—an in silico simulation study. Interact Cardiovasc Thorac Surg. 2019. https://doi.org/10.1093/icvts/ivz048.
Gates JD, Bichell DP, Rizzo RJ, Couper GS, Donaldson MC. Thigh ischemia complicating femoral vessel cannulation for cardiopulmonary bypass. Ann Thorac Surg. 1996;61:730–3.
Reddy DJ, Smith RF, Elliott JP Jr, Haddad GK, Wanek EA. Infected femoral artery false aneurysms in drug addicts: evolution of selective vascular reconstruction. J Vasc Surg. 1986;3:718–24.
Dogan S, Graubitz K, Aybek T, Khan MF, Kessler P, Moritz A, et al. How safe is the port access technique in minimally invasive coronary artery bypass grafting? Ann Thorac Surg. 2002;74:1537–43.
Dogan S, Aybeck T, Risteski PS, Detho F, Rapp A, Wimmer-Greinecker G, et al. Minimally invasive port access versus conventional mitral valve surgery: prospective randomized study. Ann Thorac Surg. 2005;79:492–8.
Vikenes K, Andersen KS, Farstad M, Nordrehaug JE. Temporal pattern of cardiac troponin I after thoracotomy and lung surgery. Int J Cardiol. 2004;96:403–7.
Acknowledgements
We are grateful to Dr. Hiroki Sato for assistance with the statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kawashima, T., Okamoto, K., Wada, T. et al. Femoral artery anatomy is a risk factor for limb ischemia in minimally invasive cardiac surgery. Gen Thorac Cardiovasc Surg 69, 246–253 (2021). https://doi.org/10.1007/s11748-020-01442-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-020-01442-y