Abstract
Purpose
The impact of perioperative heparin bridging (HB) for lung surgery in patients on anti-clotting drugs remains unclear. We performed a retrospective study to assess its effect on surgical safety by comparing HB and non-HB groups.
Methods
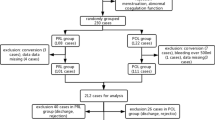
This study included 274 consecutive patients on anti-clotting drugs who underwent surgery for lung cancer. Of these, 77 received HB and 197 did not. Propensity score matching extracted 124 patients, consisting of 62 patients with HB and 62 patients without HB. Endpoints were surgical safety.
Results
There was no statistically significant difference in the outcomes of surgical safety outcomes between the HB and non-HB group after propensity-score matching, operative time (172 vs. 203 min, p = 0.131), volume of blood loss (60 vs. 70 ml, p = 0.335), need for intraoperative RBC transfusion (3.2 vs. 6.5%, p = 0.680), chest tube drainage volume on the 1st postoperative day (200 vs. 200 ml, p = 0.796), and chest tube placement duration (3 vs. 3 days, p = 0.606).
Conclusions
The influence of perioperative HB on postoperative thromboembolic or bleeding events in lung cancer surgery is not obvious, but its surgical safety appears to be acceptable.
Similar content being viewed by others
References
Daniel MW, Robby N, Nathan PC, Jack A, Anne H, Jane S, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: optimal management of anticoagulation therapy. Blood Adv. 2018;2:3257–91.
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e326S–e350S350S.
Murasaki K. Guidelines for management of anticoagulant and antiplatelet therapy in cardiovascular disease (JCS 2009). Nihon Rinsho. 2011;69(Suppl 9):567–71.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Douketis JD, Spyropoulos AC, Kaatz S, Becker RC, Caprini JA, Dunn AS, et al. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373:823–33.
Hamid G, Wouter SP, Hazim A, Rakesh L, Krit J, Thomas C, et al. Meta-analysis of safety and efficacy of uninterrupted warfarin compared to heparin-based bridging therapy during implantation of cardiac rhythm devices. Am J Cardiol. 2012;110:1482–8. https://doi.org/10.1016/j.amjcard.2012.06.057.
Rechenmacher SJ, Fang JC. Bridging anticoagulation: primum non nocere. J Am Coll Cardiol. 2015;66:1392–403.
Rose AJ, Allen AL, Minichello T. A call to reduce the use of bridging anticoagulation. Circ Cardiovasc Qual Outcomes. 2016;9:64–7. https://doi.org/10.1161/CIRCOUTCOMES.115.002430.
Marquez J, Togami JC, Dant CR, Herrera A, Marshik P, Burnett AE. Peri-procedural antithrombotic management: time to burn the bridge? J Thromb Thrombolysis. 2018;45:337–44. https://doi.org/10.1007/s11239-018-1616-3.
Ohtaka K, Hida Y, Kaga K, Iimura Y, Shiina N, Muto J, et al. Pulmonary vein thrombosis after video-assisted thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg. 2012;143:e3–e5.
Ohtaka K, Hida Y, Kaga K, Kato T, Muto J, Nakada-Kubota R, et al. Thrombosis in the pulmonary vein stump after left upper lobectomy as a possible cause of cerebral infarction. Ann Thorac Surg. 2013;95:1924–9.
Hattori A, Takamochi K, Kitamura Y, Matsunaga T, Suzuki K, Oh S, et al. Risk factor analysis of cerebral infarction and clinicopathological characteristics of left upper pulmonary vein stump thrombus after lobectomy. Gen Thorac Cardiovasc Surg. 2019;67:247–53. https://doi.org/10.1007/s11748-018-1017-8.
Yano M, Numanami H, Akiyama T, Taguchi R, Furuta C, Haniuda M. Reoperation for postoperative bleeding following pulmonary resection: a report of a single-center experience. Gen Thorac Cardiovasc Surg. 2019. https://doi.org/10.1007/s11748-018-01060-9.
Alai GH, Deng HY, Li G, Luo J, Liu LX, Lin YD. The influence of heparin on coagulation function of patients undergoing video-assisted major thoracic surgery. J Thorac Dis. 2018;10:2288–94.
Sato C, Hirasawa K, Koh R, Ikeda R, Fukuchi T, Kobayashi R, et al. Postoperative bleeding in patients on antithrombotic therapy after gastric endoscopic submucosal dissection. World J Gastroenterol. 2017;23:5557–66.
Kubo T, Yamashita K, Onodera K, Iida T, Arimura Y, Nojima M, et al. Heparin bridge therapy and post-polypectomy bleeding. World J Gastroenterol. 2016;22:10009–144.
Guglielmetti LC, Sorabella R, Chiuzan C, Najjar M, Castillero E, Lambert D, et al. Bridging anticoagulation after mechanical aortic heart valve replacement: a questionable routine. Ann Thorac Surg. 2016;102:48–544.
Childers CP, Maggard GM, Shekelle PG. Antiplatelet therapy in patients with coronary stents undergoing elective noncardiac surgery: continue, stop, or something in between? JAMA. 2017;318:120–1. https://doi.org/10.1001/jama.2017.7845.
Nagata N, Yasunaga H, Matsui H, Fushimi K, Watanabe K, Akiyama J, et al. Therapeutic endoscopy-related GI bleeding and thromboembolic events in patients using warfarin or direct oral anticoagulants: results from a large nationwide database analysis. Gut. 2018;67:1805–12. https://doi.org/10.1136/gutjnl-2017-313999.
Yanagisawa N, Nagata N, Watanabe K, Iida T, Hamada M, Kobayashi S, et al. Post-polypectomy bleeding and thromboembolism risks associated with warfarin vs direct oral anticoagulants. World J Gastroenterol. 2018;24:1540–9.
Birnie DH, Healey JS, Wells GA, Ayala-Paredes F, Coutu B, Sumner GL, et al. Continued vs. interrupted direct oral anticoagulants at the time of device surgery, in patients with moderate to high risk of arterial thrombo-embolic events (BRUISE CONTROL-2). Eur Heart J. 2018;39:3973–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest associated with this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mori, M., Ichiki, Y., Kanayama, M. et al. The impact of perioperative heparin bridging therapy in lung cancer surgery. Gen Thorac Cardiovasc Surg 68, 623–628 (2020). https://doi.org/10.1007/s11748-019-01276-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01276-3