Abstract
Background
Hypoplastic left heart syndrome is a lethal congenital heart malformation when untreated resulting in a 95% mortality in the first month of life. In this study, we aimed to investigate the newly introduced inflammatory biomarker, neutrophil–lymphocyte ratio, as a mortality predictor in postoperative hypoplastic left heart syndrome patients.
Methods
Patients were divided into two groups; Group 1 consisted of 33 patients who were discharged and Group 2 including 20 patients who were deceased following surgery. Patients’ preoperative demographic characteristics, total white blood cell counts, neutrophil counts, lymphocyte counts, neutrophil–lymphocyte ratio, C-reactive proteins, alanine aminotransferase, aspartate transaminase, urea, and creatinine levels were recorded. Studys’ primary endpoint was all-cause patient mortality following surgery.
Results
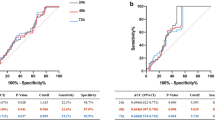
The preoperative neutrophil–lymphocyte ratio was found to be significantly different between the groups (p = 0.001). High neutrophil–lymphocyte ratio was found to be associated with an increased risk of death. The ROC curves of neutrophil–lymphocyte ratio were found to be associated with mortality. The area under curve for the preoperative neutrophil–lymphocyte ratio was 0.74. Neutrophil–lymphocyte ratio predicted mortality with a sensitivity of 78% and a specificity of 65%.
Conclusion
Neutrophil–lymphocyte ratio can contribute to the early identification of patients at high risk for complications. In addition, through the use of NLR, clinicians could implement measures for the optimal therapeutic approach of cardiac surgery patients and the elimination of adverse patient outcomes.



Similar content being viewed by others
References
Gillum R. Epidemiology of congenital heart disease in the United States. Am Heart J. 1994;127:919–27.
Feinstein JA, Benson DW, Dubin AM, et al. Hypoplastic left heart syndrome: current consideration and expectation. J Am Coll Cardiol. 2012;59:1–42.
Miller BE, Levy JH. The inflammatory response to cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 1997;11:355–66.
Butler J, Rocker MG, Westaby S. Inflammatory response to cardiopulmonary bypass. Ann Thorac Surg. 1993;55:552–59.
Khabar KSA, Elbarbary MA, Khouqueer F, et al. Circulating endotoxin and cytokines after cardiopulmonary bypass: differential correlation with duration of bypass and systemic inflammatory response/multiple organ dysfunction syndromes. Clin Immunol Immunopathol. 1997;85:97–103.
Sinden NJ, Stockley RA. Systemic inflammation and comorbidity in COPD: a result of ‘overspill’ of inflammatory mediators from the lungs? Rev Evid Thorax. 2010;65(10):930–6.
Dale DC, Boxer L, Liles WC. The phagocytes: neutrophils and monocytes. Blood. 2008;112:934–45.
Kaya H, Ertas F, Islamoglu Y, et al. Association between neutrophil to lymphocyte ratio and severity of coronary artery disease. Clin Appl Thromb Hemost. 2014;20(1):50–4.
Gibson PH, Croal BL, Cuthbertson BH, et al. Preoperative neutrophil-lymphocyte ratio and outcome from coronary artery bypass grafting. Am Heart J. 2007;154:995–1002.
Savluk OF, Guzelmeric F, Yavuz Y, et al. The neutrophil lymphocyte ratio as a successful extubation predictor of prolonged intubation in pediatric. Heart Surg. 2017;27:e9416.
Malec E, Januszewska K, Kolcz J, Pajak J. Factors influencing early outcome of Norwood procedure for hypoplastic left heart syndrome. Eur J Cardio-thorac Surg. 2000;18:202–6.
Jacobs JB, Obrien SM, Chai PJ, et al. Management of 239 patients with hypoplastic left heart syndrome and related malformation from 1993 to 2007. Ann Thorac Surg. 2008;85:1691–7.
Ashburn DA, McCrindle BW, Tchervenkov CI, et al. Outcomes after the Norwood operations in neonates with critical aortic stenosis or aortic valve atesia. J Thorac Cardiovasc Surg. 2003;125:1070–82.
Pizarro C, malec E, Maher KO. at al. Right ventricle to pulmonary artery conduit improves outcomes after stage 1 Norwood for hypoplastic left heart syndrome. Circulation. 2003;108:155–60.
Vida VL, Bacha EA, Larrazabal A, et al. Surgical outcomes for patients with the mitral stenosis-aortic atresia variant of hypoplastic left heart syndrome. J Thorac Cardiovasc Surg. 2008;135:339–46.
Kern JH, Hayes CJ, Michler RE, Gersony WM, Quaegebeur JM. Survival and risk factor analysis fort he Norwood procedure for hypoplastic left heart syndrome. Am J Cardiol. 1997;80:170–4.
Jonas RA, Hansen DD, Cook N, Wessel D. Anatomic subtype and survival after reconstructive operation for hypoplastic left heart syndrome. J Thorac Cardiovasc Surg. 1994;107:1121–8.
Daebritz SH, Nollert GD, Zurakowski D, et al. Results of Norwood stage I operations. Comparison of hypoplastic left heart syndrome with other malformations. J Thorac Cardiovasc Surg. 2000;119:358–67.
Iannettoni MD, Bove EL, Mosca RS, et al. Improving results with first-stage palliation for hypoplastic left heart syndrome. J Thorac Cardiovasc Surg. 1994;107:934–40.
Rossi AF, Sommer RJ, Steinberg LG, et al. Effect of older age on outcome for stage one palliation of hypoplastic left heart syndrome. Circulation. 1995;92:267–71.
Sano S, Huang S, Kasahara S, et al. Risk factors for mortality after the Norwood procedure using right ventricle to pulmonary artery shunt. Ann Thorac Surg. 2009;87:178–86.
Allan CK, Thigarajan R, del Nido PJ, et al. Indication for initiation of mechanical circulatory support impacts survival of infants with shunted single-ventricle circulation supported with extracorporeal membrane oxygenation. J Thorac Cardiovasc Surg. 2007;133:660–7.
Yamanaka T, Matsumoto S, Teramukai S, et al. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007;73:215–20.
Ridker PM, Rifai N, Pfeffer M, et al. Elevation of tumor necrosis factor-alpha and increased risk of recurrent coronary events after myocardial infarction. Circulation. 2000;101(18):2149–53.
Niccoli G, Montone RA, Ferrante G, et al. The evolving role of inflammatory biomarkers in risk assessment after stent implantation. J Am Coll Cardiol. 2010;56:1783–93.
Berkowitz DH, Gaynor JW. Management of pediatric cardiopulmonary bypass. In: Mayroudis C, Backer C, editors. Pediatric cardiac surgery. 4th ed. West Sussex: Wiley-Blackwell; 2013. p. 169–213.
Cabrera AG, Dyamenahalli U, Gosett J, et al. Preoperative lymphopenia is a predictor of postoperative adverse outcomes in children with congenital heart disease. J Thorac Cardiovasc Surg. 2009;138:1172–9.
Jones S, McCracken C, Alsoufi B, et al. Association of preoperative cell counts with outcomes after operation for congenital heart disease. Ann Thorac Surg. 2018;106:1234–40.
Hauser GJ, Chan MM, Casey WF, et al. Immune dysfunction in children after corrective surgery for congenital heart disease. Crit Care Med. 1991;19:874–81.
Segel GB, halterman MW, Lichtman MA. The paradox of the neutrophil’s role in tissue injury. J Leukoc Biol. 2011;89:359–72.
Cooper HA, Exner DV, Waclawiw MA, et al. White blood cell count and mortality in patients with ischemic and nonischemic left ventricular systolic dysfunction (an analysis of the Studies of left Ventricular Dysfunction (SOLVD)). Am J Cardiol. 1999;84:252–7.
Gurm HS, Bhatt DL, Lincoff AM, et al. Impact of preprocedural white blood cell count on long term mortality after percutaneous coronary intervention: insights from the EPIC, EPILOG and EPISTENT trials. Heart. 2003;89:1200–4.
Bocsi J, Hambsch J, Osmancik P, et al. Preoperative prediction of pediatric patients with effusions and edema following cardiopulmonary bypass surgery by serological and routine laboratory data. Crit Care. 2002;6:226–33.
Guasti L, Dentali F, Castiglioni L, et al. Neutrophils and clinical outcomes in patients with acute coronary syndromes and/or cardiac revascularization. A systematic review on more than 34,000 subjects. Thromb Haemost. 2011;106:591–9.
Appachi E, Mossad E, Mee R, et al. Perioperative serum interleukins in neonates with hypoplastic left heart syndrome and transposition of the great arteries. J Cardiothoracic Vasc Anesth. 2007;21(2):184–90.
Mitchell E, Chetham J, Sisk J, et al. Neutrophil Lymphocyte ratio and association with arch intervention in patients with hypoplastic left heart syndrome undergoing hybrid procedure. Congenit Heart Dis. 2014;9(6):543–8.
Hartaigh B, Bosch JA, Thomas GN, et al. Which leukocyte subsets predict cardiovascular mortality? From the Ludwingshafen risk And Cardiovascular Health(LURIC) study. Atherosclerosis. 2012;224:161–9.
Sawant AC, Adhikari P, Narra SR, et al. Neutrophil to lymphocyte ratio predicts short and long term mortality following revascularization therapy for ST elevation myocardial infarction. Cardiol J. 2014;21:500–8.
Silberman S, Abu-Yunis U, BMed SCi, et al. Neutrophil–lymphocyte ratio: prognostic impact in heart surgery. Early outcomes and late survival. Ann Thorac Surg. 2018;105:581–6.
Major AS, Fazio S, Linton MF. B-lymphocyte deficiency increases atherosclerosis in LDL receptor-null mice. Arterioscler Thromb Vasc Biol. 2002;22:1892–8.
Nunez J, Sanchis J, Bodi V, et al. Relationship between low lymphocyte counts and major cardiac events in patients with acute chest pain, a non-diagnostic electrocardiogram and normal troponin levels. Atherosclerosis. 2009;206:251–7.
Gursoy M, Salihoglu E, Hatemi AC, et al. Inflammation and congenital heart disease associated pulmonary hypertension. Heart Surg Forum. 2015;18(1):E38–41.
Bagger JP, Zindrou D, Taylor KM. Leukocyte count: a risk factor for coronary artery bypass graft mortality. Am J Med. 2003;115:660–3.
Newal N, Grayson AD, Oo AY, et al. Preoperative white blood cell count is independently associated with higher perioperative cardiac enzyme release and increased 1-year mortality after coronary artery bypass grafting. Ann Thorac Surg. 2006;81:583–9.
Demir M. The relationship between neutrophil lymphocyte ratio and non-dipper hypertension. Clin Exp Hypertens. 2013;35(8):570–3.
Suliman M, Juma B, Almadhani A, et al. Predictive value of neutrophil to lymphocyte ratio in outcomes of patients with acute coronary syndrome. Arch Med Res. 2010;41(8):618–22.
Nunez J, Nunez E, Minana G, et al. Effectiveness of the relative lymphocyte count to predict one-year mortality in patients with acute heart failure. Am J Cardiol. 2011;107(7):1034–9.
Uthamalingam S, Patvardhan EA, Subramanian, et al. Utility of the neutrophil to lymphocyte ratio in predicting long-term outcomes in acute decompensates heart failure. Am J Cardiol. 2011;107(3):433–38.
Funding
No financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Savluk, O.F., Guzelmeric, F., Yavuz, Y. et al. Neutrophil–lymphocyte ratio as a mortality predictor for Norwood stage I operations. Gen Thorac Cardiovasc Surg 67, 669–676 (2019). https://doi.org/10.1007/s11748-019-01081-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01081-y