Abstract
Background
Limited information is currently available on the postoperative outcomes of Mycobacterium avium complex lung disease (MAC-LD).
Objective
To show the outcomes of pulmonary resection and identify risk factors after adjuvant surgical treatments for MAC-LD.
Methods
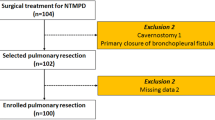
One hundred and eight patients underwent adjuvant lung resection for MAC-LD at two hospitals between January 2008 and July 2016. We retrospectively evaluated outcomes and risk factors.
Results
Postoperative complications occurred in 14 patients (13%). After lung resection, 98 out of 108 patients (91%) achieved sputum culture conversion, eight (8.2%) of whom developed microbiological recurrence during the follow-up period. As a result, the success rate of adjuvant surgical treatments for MAC-LD with drug resistance was 83%. A multivariable analysis showed that a longer period from the initial medical treatment to surgery (hazard ratio, 1.01; 95% confidence interval, 1.00–1.02; p = 0.008) was independently associated with an increased risk of unfavorable outcomes after adjuvant surgery.
Conclusions
Adjuvant surgical treatments for MAC-LD have acceptable outcomes. Better control of the disease may be achieved in some patients with drug resistance and indications for surgery through surgical treatments, and pulmonary resection needs to be performed earlier rather than continuing chemotherapy in these patients because it reduces unfavorable outcomes.


Similar content being viewed by others
References
Prevots DR, Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin Chest Med. 2015;36:13–34.
Namkoong H, Kurashima A, Morimoto K, Hoshino Y, Hasegawa N, Ato M, et al. Epidemiology of pulmonary nontuberculous mycobacterial disease, Japan (1). Emerg Infect Dis. 2016;22:1116–7.
Field SK, Fisher D, Cowie RL. Mycobacterium avium complex pulmonary disease in patients without HIV infection. Chest. 2004;126:566–81.
Kobashi Y, Matsushima T, Oka M. A double-blind randomized study of aminoglycoside infusion with combined therapy for pulmonary Mycobacterium avium complex disease. Respir Med. 2007;101:130–8.
Koh WJ, Jeong BH, Jeon K, Lee NY, Lee KS, Woo SY, et al. Clinical significance of the differentiation between Mycobacterium avium and Mycobacterium intracellulare in M. avium complex lung disease. Chest. 2012;142:1482–8.
Xu HB, Jiang RH, Li L. Treatment outcomes for Mycobacterium avium complex: a systematic review and meta-analysis. Eur J Clin Microbiol Infect Dis. 2014;33:347–58.
Shiraishi Y, Katsuragi N, Kita H, Hyogotani A, Saito MH, Shimoda K. Adjuvant surgical treatment of nontuberculous mycobacterial lung disease. Ann Thorac Surg. 2013;96:287–91.
Kang HK, Park HY, Kim D, Jeong BH, Jeon K, Cho JH, et al. Treatment outcomes of adjuvant resectional surgery for nontuberculous mycobacterial lung disease. BMC Infect Dis. 2015;15:76.
Runyon EH. Mycobacterium intracellulare. Am Rev Respir Dis. 1967;95:861–5.
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al, ATS Mycobacterial Diseases Subcommittee; American Thoracic Society; Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367–416.
Park YS, Lee CH, Lee SM, Yang SC, Yoo CG, Kim YW, et al. Rapid increase of non-tuberculous mycobacterial lung diseases at a tertiary referral hospital in South Korea. Int J Tuberc Lung Dis. 2010;14:1069–71.
Prevots DR, Shaw PA, Strickland D, Jackson LA, Raebel MA, Blosky MA, et al. Nontuberculous mycobacterial lung disease prevalence at four integrated health care delivery systems. Am J Respir Crit Care Med. 2010;182:970–6.
Hayashi M, Takayanagi N, Kanauchi T, Miyahara Y, Yanagisawa T, Sugita Y. Prognostic factors of 634 HIV-negative patients with Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2012;185:575–83.
Markos J, Mullan BP, Hillman DR, Musk AW, Antico VF, Lovegrove FT, et al. Preoperative assessment as a predictor of mortality and morbidity after lung resection. Am Rev Respir Dis. 1989;139:902–10.
Wallace RJ Jr, Brown-Elliott BA, McNulty S, Philley JV, Killingley J, Wilson RW, et al. Macrolide/Azalide therapy for nodular/bronchiectatic Mycobacterium avium complex lung disease. Chest. 2014;146:276–82.
Kanda y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Mitchell JD, Bishop A, Cafaro A, Weyant MJ, Pomerantz M. Anatomic lung resection for nontuberculous mycobacterial disease. Ann Thorac Surg. 2008;85:1887–92.
Yu JA, Pomerantz M, Bishop A, Weyant MJ, Mitchell JD. Lady Windermere revisited: treatment with thoracoscopic lobectomy/segmentectomy for right middle lobe and lingular bronchiectasis associated with non-tuberculous mycobacterial disease. Eur J Cardiothorac Surg. 2011;40:671–5.
Mitchell JD, Yu JA, Bishop A, Weyant MJ, Pomerantz M. Thoracoscopic lobectomy and segmentectomy for infectious lung disease. Ann Thorac Surg. 2012;93:1033–9.
Asakura T, Hayakawa N, Hasegawa N, Namkoong H, Takeuchi K, Suzuki S, et al. Long-term outcome of pulmonary resection for nontuberculous mycobacterial pulmonary disease. Clin Infect Dis. 2017;65:244–51.
Kwak N, Park J, Kim E, Lee CH, Han SK, Yim JJ. Treatment outcomes of Mycobacterium avium complex lung disease: a systematic review and meta-analysis. Clin Infect Dis. 2017;65:1077–84.
Lee BY, Kim S, Hong YoonKi, Lee S-D, Kim WS, Kim DS, et al. Risk factors for recurrence after successful treatment of Mycobacterium avium complex lung disease. Antimicrob Agents Chemother. 2015;59:2972–7.
Okumura M, Iwai K, Ogata H, Ueyama M, Kubota M, Aoki M, et al. Clinical factors on cavitary and nodular bronchiectatic types in pulmonary Mycobacterium avium complex disease. Intern Med. 2008;47:1465–72.
Acknowledgements
We thank Akiko Kada and Noriko Ito for their helpful advice on statistical methods.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Rights and permissions
About this article
Cite this article
Yamada, K., Seki, Y., Nakagawa, T. et al. Outcomes and risk factors after adjuvant surgical treatments for Mycobacterium avium complex lung disease. Gen Thorac Cardiovasc Surg 67, 363–369 (2019). https://doi.org/10.1007/s11748-018-1029-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-018-1029-4