Abstract
Objective
Current techniques for mitral valve repair (MVR) in Barlow’s disease require high level of surgical expertise due to a complex anatomy. A novel and simple standardized technique that particularly considers the pathological changes of the mitral valve in Barlow’s disease has been developed.
Methods
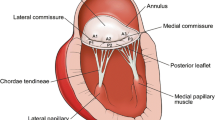
Between 2009 and 2013, 22 patients underwent minimally invasive MVR for Barlow’s disease and severe mitral regurgitation (MR). A simple, standardized technique was applied, including resection of P2 segment of posterior mitral leaflet (PML) with preservation of the shortest chordae, transfer of the preserved chordae to A2, and implantation of a semi-rigid open ring. In 2015, all patients were contacted for follow-up by transthoracic echocardiography (TTE) and interviewed for their clinical status.
Results
During follow-up (mean 2.8 ± 1.1 years; 100% complete), one patient died due to abdominal bleeding 4 months after the initial MVR and one patient with severe calcification of PML underwent valve replacement due to recurrence of MR. Among the remaining cohort (mean follow-up 3.0 ± 1.0 years), NYHA class I, II and III was present in 13, 6, and 1, respectively. TTE demonstrated MR grade 0, 1+, or 2+ in 40, 55, and 5%, respectively, with mean and maximum transvalvular gradients ranging at 1.9 ± 1.7 and 4.7 ± 3.3 mmHg, respectively.
Conclusions
A simple and standardized technique facilitates the repair of MR in the presence of Barlow’s, simultaneously addressing the height of PML and the position of the anterior leaflet. This technique has proven durable in the mid-term follow-up in our small series and warrants further validation in larger cohorts.



Similar content being viewed by others
References
Barlow JB, Bosman CK. Aneurysmal protrusion of the posterior leaflet of the mitral valve. An auscultatory-electrocardiographic syndrome. Am Heart J. 1966;71:166–78.
Miura T, Ariyoshi T, Tanigawa K, et al. Technical aspects of mitral valve repair in Barlow’s valve with prolapse of both leaflets: triangular resection for excess tissue, sophisticated chordal replacement, and their combination (the restoration technique). General thorac Cardiovasc Surg. 2015;63:61–70.
Borger MA, Kaeding AF, Seeburger J, et al. Minimally invasive mitral valve repair in Barlow’s disease: early and long-term results. J Thorac Cardiovasc Surg. 2014;148:1379–85.
Melnitchouk SI, Seeburger J, Kaeding AF, Misfeld M, Mohr FW, Borger MA. Barlow’s mitral valve disease: results of conventional and minimally invasive repair approaches. Annals Cardiothorac Surg. 2013;2:768–73.
Shibata T. Loop technique for mitral valve repair. General thorac Cardiovasc Surg. 2014;62:71–7.
da Rocha ESJG, Spampinato R, Misfeld M, et al. Barlow’s mitral valve disease: a comparison of neochordal (loop) and edge-to-edge (alfieri) minimally invasive repair techniques. Ann Thorac Surg. 2015;100:2127–33 (discussion 2133-5).
Enriquez-Sarano M, Akins CW, Vahanian A. Mitral regurgitation. Lancet. 2009;373:1382–94.
Nishimura RA, Otto CM, Bonow RO et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 2014;148:e1–132.
Miura T, Eishi K, Yamachika S, et al. Systolic anterior motion after mitral valve repair: predicting factors and management. General thoracic cardiovascular surgery. 2011;59:737–42.
Varghese R, Itagaki S, Anyanwu AC, Trigo P, Fischer G, Adams DH. Predicting systolic anterior motion after mitral valve reconstruction: using intraoperative transoesophageal echocardiography to identify those at greatest risk. Eur J Cardiothorac Surg. 2014;45:132–7 (discussion 137-8).
Adams DH, Anyanwu AC, Rahmanian PB, Abascal V, Salzberg SP, Filsoufi F. Large annuloplasty rings facilitate mitral valve repair in Barlow’s disease. Ann Thorac Surg. 2006;82:2096–100 (discussion 2101).
Kuntze T, Borger MA, Falk V, et al. Early and mid-term results of mitral valve repair using premeasured Gore-Tex loops (‘loop technique’). Eur J Cardiothorac Surg. 2008;33:566–72.
Ibrahim M, Rao C, Savvopoulou M, Casula R, Athanasiou T. Outcomes of mitral valve repair using artificial chordae. Eur J Cardiothorac Surg. 2014;45:593–601.
Perier P, Hohenberger W, Lakew F, et al. Toward a new paradigm for the reconstruction of posterior leaflet prolapse: midterm results of the “respect rather than resect” approach. Ann Thorac Surg. 2008;86:718–25. (discussion 718–25).
Lawrie GM, Earle EA, Earle NR. Nonresectional repair of the barlow mitral valve: importance of dynamic annular evaluation. Ann Thorac Surg. 2009;88:1191–6.
Maisano F, Schreuder JJ, Oppizzi M, Fiorani B, Fino C, Alfieri O. The double-orifice technique as a standardized approach to treat mitral regurgitation due to severe myxomatous disease: surgical technique. Eur J Cardiothorac Surg. 2000;17:201–5.
Acknowledgements
The authors are grateful for the support of Hildegard Gramsch-Zabel regarding echocardiographic evaluation and interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest to declare.
Additional information
H. Kamiya and P. Akhyari contributed equally to this article.
Rights and permissions
About this article
Cite this article
Kamiya, H., Akhyari, P., Minol, JP. et al. Simple technique of repair for Barlow syndrome with posterior resection and chordal transfer via minimally invasive approach: primary experience in a consecutive series of 22 patients. Gen Thorac Cardiovasc Surg 65, 374–380 (2017). https://doi.org/10.1007/s11748-017-0767-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-017-0767-z