Abstract
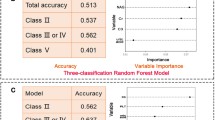
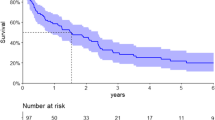
To develop a more accurate prognostic model that incorporates indicators of multi-organ involvement for immunoglobulin light-chain (AL) Amyloidosis patients. Biopsy-proven AL amyloidosis patients between January 1, 2012, and February 28, 2023, were enrolled and randomly divided into a training set and a test set at a ratio of 7:3. Prognostic indicators that comprehensively cover cardiac, renal, and hepatic involvement were identified in the training set by random survival forest (RSF). Then, RSF and Cox models were established. The Concordance index (C-index) and integrated brier scores (IBS) were applied to evaluate the models’ performance in the test set. Besides, the net reclassification index (NRI) and integrated discrimination improvement (IDI) were calculated. A total of 173 eligible patients were included. After a median follow-up of 25.9 (9.2, 50.3) months, 48 (27.7%) patients died. Creatine kinase-MB, estimated glomerular filtration rate ≤ 50 mL/min/1.73 m2, interventricular septum ≥ 15 mm, ejection fraction, alanine aminotransferase and Live involved were selected to develop prediction models. The RSF model based on the above indicators achieved C-index and IBS values of 0.834 (95% CI 0.725–0.915) and 0.151 (95% CI 0.1402–0.181), respectively. At last, the NRI and IDI of the RSF model were 0.301 (95% CI 0.048–0.546, P = 0.012) and 0.157 (95% CI 0.041–0.269, P < 0.001) at 5-year by comparing the RSF model with the Cox model which is based on the Mayo 2012 staging system. The RSF model that incorporates indicators of multi-organ involvement had a great performance, which may be helpful for physicians’ decision-making and more accurate overall survival prediction.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Zanwar S, Gertz MA, Muchtar E (2023) Immunoglobulin light chain amyloidosis: diagnosis and risk assessment. J Natl Compr Canc Netw 21(1):83–90
Quock TP et al (2018) Epidemiology of AL amyloidosis: a real-world study using US claims data. Blood Adv 2(10):1046–1053
Kumar N et al (2022) Global epidemiology of amyloid light-chain amyloidosis. Orphanet J Rare Dis 17(1):278
Staron A et al (2021) Marked progress in AL amyloidosis survival: a 40-year longitudinal natural history study. Blood Cancer J 11(8):139
Palladini G et al (2023) The management of light chain (AL) amyloidosis in Europe: clinical characteristics, treatment patterns, and efficacy outcomes between 2004 and 2018. Blood Cancer J 13(1):19
Muchtar E et al (2017) Improved outcomes for newly diagnosed AL amyloidosis between 2000 and 2014: cracking the glass ceiling of early death. Blood 129(15):2111–2119
Kumar S et al (2012) Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol 30(9):989–995
Oubari S et al (2024) Daratumumab in first-line treatment of patients with light chain amyloidosis and Mayo stage IIIb improves treatment response and overall survival. Haematologica 109(1):220–230
Kastritis E et al (2021) Daratumumab-based treatment for immunoglobulin light-chain amyloidosis. N Engl J Med 385(1):46–58
Wechalekar AD et al (2023) Guidelines for non-transplant chemotherapy for treatment of systemic AL amyloidosis: EHA-ISA working group. Amyloid 30(1):3–17
Khwaja J et al (2024) Limited utility of Mayo 2012 cardiac staging system for risk stratification of patients with advanced cardiac AL amyloidosis - analysis of a uniformly treated cohort of 1,275 patients. Haematologica. https://doi.org/10.3324/haematol.2023.284348
Fotiou D, Theodorakakou F, Kastritis E (2021) Biomarkers in AL amyloidosis. Int J Mol Sci 22(20):10916
Jamet B et al (2021) Random survival forest to predict transplant-eligible newly diagnosed multiple myeloma outcome including FDG-PET radiomics: a combined analysis of two independent prospective European trials. Eur J Nucl Med Mol Imaging 48(4):1005–1015
Bohannan ZS, Coffman F, Mitrofanova A (2022) Random survival forest model identifies novel biomarkers of event-free survival in high-risk pediatric acute lymphoblastic leukemia. Comput Struct Biotechnol J 20:583–597
Rajkumar SV et al (2014) International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 15(12):e538–e548
Gertz MA et al. (2005) Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18–22 Apr 2004. pp. 319–328
Collins GS et al (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ (Clin Res Ed) 350:g7594
Garcia-Garcia HM et al (2019) Impact of periprocedural myocardial biomarker elevation on mortality following elective percutaneous coronary intervention. JACC Cardiovasc Interv 12(19):1954–1962
Jang JG et al (2020) Prognostic factors for severe coronavirus disease 2019 in Daegu, Korea. J Korean Med Sci 35(23):e209
Brenner DA et al (2004) Human amyloidogenic light chains directly impair cardiomyocyte function through an increase in cellular oxidant stress. Circ Res 94(8):1008–1010
Ghio S et al (2007) Importance of the echocardiographic evaluation of right ventricular function in patients with AL amyloidosis. Eur J Heart Fail 9(8):808–813
Wang X et al (2022) Feasibility of (68)Ga-labeled fibroblast activation protein inhibitor PET/CT in light-chain cardiac amyloidosis. JACC Cardiovasc Imaging 15(11):1960–1970
Gertz MA, Kyle RA (1988) Hepatic amyloidosis (primary [AL], immunoglobulin light chain): the natural history in 80 patients. Am J Med 85(1):73–80
Park MA et al (2003) Primary (AL) hepatic amyloidosis: clinical features and natural history in 98 patients. Medicine 82(5):291–298
Rosenzweig M, Kastritis E (2020) Liver and gastrointestinal involvement: update. Hematol Oncol Clin North Am 34(6S):e1–e13
Borovac JA et al (2020) Right ventricular free wall strain and congestive hepatopathy in patients with acute worsening of chronic heart failure: a CATSTAT-HF echo substudy. J Clin Med 9(5):1317
Migrino RQ et al (2009) Left ventricular ejection time on echocardiography predicts long-term mortality in light chain amyloidosis. J Am Soc Echocardiogr 22(12):1396–1402
Dittrich T et al (2019) Performance analysis of AL amyloidosis cardiac biomarker staging systems with special focus on renal failure and atrial arrhythmia. Haematologica 104(7):1451–1459
Palladini G et al (2014) A staging system for renal outcome and early markers of renal response to chemotherapy in AL amyloidosis. Blood 124(15):2325–2332
Jimenez-Zepeda V et al (2023) A comprehensive multidisciplinary diagnostic algorithm for the early and efficient detection of amyloidosis. Clin Lymphoma Myeloma Leuk 23(3):194–202
Yan W et al (2021) A prognostic staging system for light-chain amyloidosis using hepatic and renal indicator data from 1,064 Chinese patients. Ann Transl Med 9(16):1347–1347
Taylor JMG (2011) Random survival forests. J Thorac Oncol 6(12):1974–1975
Dispenzieri A et al (2003) Survival in patients with primary systemic amyloidosis and raised serum cardiac troponins. Lancet 361(9371):1787–1789
Palladini G et al (2010) The combination of high-sensitivity cardiac troponin T (hs-cTnT) at presentation and changes in N-terminal natriuretic peptide type B (NT-proBNP) after chemotherapy best predicts survival in AL amyloidosis. Blood 116(18):3426–3430
Kumar S et al (2023) Impact of cytogenetic abnormalities on treatment outcomes in patients with amyloid light-chain amyloidosis: subanalyses from the ANDROMEDA study. Amyloid 30(3):268–278
Chakraborty R et al (2023) First report of outcomes in patients with stage IIIb AL amyloidosis treated with Dara-VCD front-line therapy. Br J Haematol 201(5):913–916
Acknowledgements
The authors would like to acknowledge all statisticians for participating in this study.
Funding
This work was supported by the National Natural Science Foundation of China (grants number 82170722, 82270715), Key Research and Development Plan of Shaanxi Province (grants number No.2023-ZDLSF-15), Research topic of clinical application of military medicine in Xijing Hospital (Reference number: JSYYZ05), Clinical research project of Fourth Military Medical University (grants number 2021LC2205), and Postdoctoral Lan Jian Sustentation Fund of the Fourth Military Medical University (grants number lj20220102).
Author information
Authors and Affiliations
Contributions
Y. Xing and S. Sun: Conceptualization; Y. Xing, and J. Zhao: Methodology; X. Li and W. Zheng: Data curation; X. Li and Y. Xing: Writing- Original draft preparation; Y. Xing, X. Li, H. Wu and L. Zhao: Visualization and Supervision. S. Sun: Validation and Writing- Reviewing and Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xing, Y., Li, X., Zhao, J. et al. Advancing precision medicine in immunoglobulin light-chain amyloidosis: a novel prognostic model incorporating multi-organ indicators. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03621-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03621-8