Abstract
Background
The aim of our study was to evaluate the impact of an internist physician specialized in diabetes, appointed as an in-house physician in the orthopedic wards, on improving clinical outcomes and in particular 30-day mortality.
Methods
We analyzed a cohort of patients hospitalized more than 24 h in the orthopedic service. The analyses included a comparative analysis between the pre- and post-intervention time periods and an interrupted time series (ITS) analysis, which were conducted in stratification to three populations: whole population, patients with at least one chronic disease and/or older than 75 years of age and patients diagnosed with diabetes. The primary outcome was 30-day mortality following the hospitalization.
Results
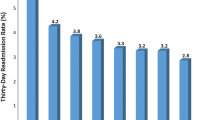
A total of 11,546 patients were included in the study, of which 19% (2212) were hospitalized in the post intervention period. Although in the comparative analysis there was no significant change in 30-day mortality, in the ITS there was a decrease in the mortality trend during the post intervention period in the entire and chronic disease/elderly populations, compared to no change during the pre-intervention period: a post-intervention slope of − 0.14(p value < 0.001) and − 0.11(p value = 0.03), respectively. Additionally, we found decrease in length of stay, increase in transfers to the internal medicine department with a negative trend, increase in HbA1c testing during the hospitalization and changes in diabetes drugs administration.
Conclusion
The presence of an internist in the orthopedic wards is associated with health care improvement; decrease in the 30-day mortality trend, decrease in length of stay, increase in HbA1c testing during the hospitalization and an increase in diabetes drugs administration.

Similar content being viewed by others
References
Batsis JA, Phy MP, Melton LJ et al (2007) Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med 2:219–225. https://doi.org/10.1002/jhm.207
Rocca GJD, Moylan KC, Crist BD et al (2013) Comanagement of geriatric patients with hip fractures: a retrospective, controlled, cohort study. Geriatr Orthop Surg Rehabil 4:10–15. https://doi.org/10.1177/2151458513495238
Folbert ECE, Smit RS, van der Velde D et al (2012) Geriatric fracture center: a multidisciplinary treatment approach for older patients with a hip fracture improved quality of clinical care and short-term treatment outcomes. Geriatr Orthop Surg Rehabil 3:59–67. https://doi.org/10.1177/2151458512444288
Friedman SM, Mendelson DA, Kates SL, McCann RM (2008) Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc 56:1349–1356
Kates SL, Blake D, Bingham KW et al (2010) Comparison of an organized geriatric fracture program to united states government data. Geriatr Orthop Surg Rehabil 1:15–21. https://doi.org/10.1177/2151458510382231
Kates SL, Mendelson DA, Friedman SM (2010) Co-managed care for fragility hip fractures (Rochester model). Osteoporos Int 21(4):621–625
Miura LN, Dipiero AR, Homer LD (2009) Effects of a geriatrician-led hip fracture program: improvements in clinical and economic outcomes. J Am Geriatr Soc 57:159–167. https://doi.org/10.1111/j.1532-5415.2008.02069.x
Phy MP, Vanness DJ, Melton LJ et al (2005) Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med 165:796–801. https://doi.org/10.1001/archinte.165.7.796
The impact of hospitalists on length of stay and costs: systematic review and meta-analysis - PubMed. https://pubmed-ncbi-nlm-nih-gov.ezproxy.bgu.ac.il/22435787/. Accessed 4 Feb 2021
Schnell S, Friedman SM, Mendelson DA et al (2010) The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil 1:6–14. https://doi.org/10.1177/2151458510378105
Friedman SM, Mendelson DA, Bingham KW, Kates SL (2009) Impact of a comanaged geriatric fracture center on short-term hip fracture outcomes. Arch Intern Med 169:1712–1717. https://doi.org/10.1001/archinternmed.2009.321
PausJenssen L, Ward HA, Card SE (2008) An internist’s role in perioperative medicine: a survey of surgeons’ opinions. BMC Fam Pract. https://doi.org/10.1186/1471-2296-9-4
Shaw M, Pelecanos AM, Mudge AM (2020) Evaluation of internal medicine physician or multidisciplinary team comanagement of surgical patients and clinical outcomes: a systematic review and meta-analysis. JAMA Netw open 3:e204088. https://doi.org/10.1001/jamanetworkopen.2020.4088
Jiao H, Xiao E, Graves DT (2015) Diabetes and its effect on bone and fracture healing. Curr Osteoporos Rep 13:327–335
Stolarczyk A, Sarzyńska S, Gondek A, Cudnoch-Jędrzejewska A (2018) Influence of diabetes on tissue healing in orthopaedic injuries. Clin Exp Pharmacol Physiol 45:619–627
Jin J, Wang Y, Deng Z (2017) Increased risk of diabetes in inflammatory orthopedics diseases. AME Med J. https://doi.org/10.21037/amj.2017.05.25
Hong CK, Chang CJ, Kuan FC et al (2020) Patients with diabetes mellitus have a higher risk of tendon retear after arthroscopic rotator cuff repair a meta-analysis. Orthop J Sport Med. https://doi.org/10.1177/2325967120961406
Lecka-Czernik B (2017) Diabetes, bone and glucose-lowering agents: basic biology. Diabetologia 60:1163–1169
Veronese N, Cooper C, Reginster JY et al (2019) Type 2 diabetes mellitus and osteoarthritis. Semin Arthritis Rheum 49:9–19
Grossman DC, Bibbins-Domingo K, Curry SJ et al (2017) Screening for obesity in children and adolescents us preventive services task force recommendation statement. JAMA 317:2417–2426. https://doi.org/10.1001/jama.2017.6803
Diamond HS, Goldberg E, Janosky JE (1998) The effect of full-time faculty hospitalists on the efficiency of care at a community teaching hospital. Ann Intern Med 129:197–203. https://doi.org/10.7326/0003-4819-129-3-199808010-00006
Folbert EC, Hegeman JH, Vermeer M et al (2017) Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int 28:269–277. https://doi.org/10.1007/s00198-016-3711-7
Craig P, Dieppe P, Macintyre S et al (2008) Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 337:979–983
Bernal JL, Cummins S, Gasparrini A (2017) Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 46:348–355. https://doi.org/10.1093/ije/dyw098
Soumerai SB, Starr D, Majumdar SR (2015) How do you know which health care effectiveness research you can trust? A guide to study design for the perplexed. Prev Chronic Dis. https://doi.org/10.5888/pcd12.150187
Sharma G, Kuo YF, Freeman J et al (2010) Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med 170:363–368. https://doi.org/10.1001/archinternmed.2009.553
Co-Management of Surgical Patients - ProQuest. https://www-proquest-com.ezproxy.bgu.ac.il/docview/1540478536?accountid=14484. Accessed 8 Feb 2021
Wachter RM, Goldman L (1996) The Emerging role of “hospitalists” in the american health care system. N Engl J Med 335:514–517. https://doi.org/10.1056/nejm199608153350713
Auerbach AD, Rasic MA, Sehgal N et al (2007) Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med 167:2338–2344. https://doi.org/10.1001/archinte.167.21.2338
Chuang CH, Pinkowsky GJ, Hollenbeak CS, Armstrong AD (2010) Medicine versus orthopaedic service for hospital management of hip fractures. Clin Orthop Relat Res 468:2218–2223. https://doi.org/10.1007/s11999-010-1290-z
Duplantier NL, Briski DC, Luce LT et al (2016) The effects of a hospitalist comanagement model for joint arthroplasty patients in a teaching facility. J Arthroplasty 31:567–572. https://doi.org/10.1016/j.arth.2015.10.010
Sharma G (2014) Medical consultation for surgical cases in the era of value-based care. JAMA Intern Med 174:1477–1478
Kammerlander C, Roth T, Friedman SM et al (2010) Ortho-geriatric service—a literature review comparing different models. Osteoporos Int 21(4):637–646
Van Grootven BV, Flamaing J, De Casterlé BD et al (2017) Effectiveness of in-hospital geriatric co-management: a systematic review and meta-analysis. Age Ageing 46:903–910. https://doi.org/10.1093/ageing/afx051
Wang H, Li C, Zhang Y et al (2015) The influence of inpatient comprehensive geriatric care on elderly patients with hip fractures: a meta-analysis of randomized controlled trials. Int J Clin Exp Med 8:19815–19830
Diabetes care in the hospital (2018) Standards of medical care in Diabetesd. Diabetes Care 41:S144–S151. https://doi.org/10.2337/dc18-S014
Strack B, Deshazo JP, Gennings C et al (2014) Impact of HbA1c measurement on hospital readmission rates: Analysis of 70,000 clinical database patient records. Biomed Res Int. https://doi.org/10.1155/2014/781670
Wu EQ, Zhou S, Yu A et al (1995) (2012) Outcomes associated with post-discharge insulin continuity in US patients with type 2 diabetes mellitus initiating insulin in the hospital. Hosp Pract 40:40–48. https://doi.org/10.3810/hp.2012.10.1002
Umpierrez GE, Reyes D, Smiley D et al (2014) Hospital discharge algorithm based on admission HbA1c for the management of patients with type 2 diabetes. Diabetes Care 37:2934–2939. https://doi.org/10.2337/dc14-0479
Author information
Authors and Affiliations
Contributions
SS: substantial contributions to the design of the work and writing, VP: substantial contributions to the conception of the work and writing, TF: substantively revised the work and approved it.
Corresponding author
Ethics declarations
Conflict of interest:
The authors declare that they have no competing interests
Research involving human and animal participant
The research shows that a diabetes specialized internist embedded in an orthopedic service is associated with health care improvements for the elderly population; decrease in the 30-day mortality trend, decrease in LOS, increase in HbA1c testing during the hospitalization and increase in diabetes drugs administration.
Informed consent
For this type of study no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shashar, S., Polischuk, V. & Friesem, T. Internal medicine physician embedded in an orthopedic service in a level 1 hospital: clinical impact. Intern Emerg Med 17, 339–348 (2022). https://doi.org/10.1007/s11739-021-02745-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-021-02745-5