Abstract
Objective
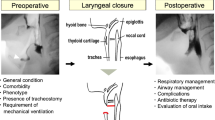
To observe the clinical efficacy of fire-needle therapy in treating deglutition disorders due to pseudobulbar palsy in the remission stage of stroke.
Methods
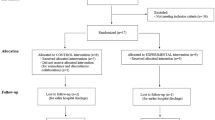
Sixty-two eligible subjects were divided into a fire-needle group and a rehabilitation group by a simple randomization method at a ratio of 1:1. The two groups received same basic intervention; in addition, the fire-needle group received fire-needle treatment, while the rehabilitation group received rehabilitation training. The two groups of subjects all received a 3-week treatment and were evaluated by the dysphagia severity rating scale (DSRS), modified Mann assessment of swallow ability (MMASA) and Kubota Toshio swallow test (KTST) before and after the intervention. The complications and adverse events occurred during the trial were recorded. The data were statistically analyzed.
Results
At the third week, the DSRS, MMASA and KTST scores changed significantly compared with the baseline in both groups (P<0.05), and the changes in the fire-needle group were more significant than those in the rehabilitation group (P<0.05). The between-group comparison at the third week showed that the therapeutic efficacy in the fireneedle group was superior to that in the rehabilitation group (P<0.05).
Conclusion
Fire-needle therapy can obviously change the DSRS, MMASA and KTST scores in pseudobulbar palsy in the remission stage of stroke, and significantly enhance the therapeutic efficacy of the treatment of deglutition disorders in this stage.
摘要
目的
观察火针治疗卒中恢复期假性延髓麻痹吞咽困难的临床疗效。
方法
将符合纳入标准的62例受试者按1:1比例采用简单随机法分为火针组和康复组。两组接受相同的基础治疗, 火针组加用火针治疗, 康复组加用 康复训练。两组受试者均治疗3周, 分别在治疗前、治疗后进行吞咽严重程度量表(DSRS)、改良版Mann吞咽量表 (MMASA)和洼田俊夫饮水测试(KTST)三个量表的评价, 并对实验过程中的并发症、不良反应等进行记录, 最后对研究数据进行统计学分析。
结果
在第3周, 两组DSRS、MMASA和KTST与治疗前比较有显著改变(P<0.05), 且火针组与康复组比较差异显著(P<0.05)。在第3周时两组间疗效比较, 火针组疗效均优于康复组(P<0.05)。
结论
火针可以显著改变卒中恢复期假性延髓麻痹的DSRS、MMASA和KTST评分, 显著提高卒中恢复期假性延髓麻痹吞咽困难的疗效。
Similar content being viewed by others
References
Fedder WN. Review of evidenced-based nursing protocols for dysphagia assessment. Stroke, 2017, 48(4): e99–e101.
Cohen DL, Roffe C, Beavan J, Blackett B, Fairfield CA, Hamdy S, Havard D, McFarlane M, McLauglin C, Randall M, Robson K, Scutt P, Smith C, Smithard D, Sprigg N, Warusevitane A, Watkins C, Woodhouse L, Bath PM. Post-stroke dysphagia: a review and design considerations for future trials. Int J Stroke, 2016, 11(4): 399–411.
Collaborative Group of Acute Encephalopathy of State Administration of Traditional Chinese Medicine. Standard for diagnosis and therapeutic effect evaluation of stroke (trial). Beijing Zhongyiyao Daxue Xuebao, 1996, 19(1): 55–56.
Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379–380.
Pourmand R. Practicing Neurology. New Jersey: Humana Press, 2008: 42.
Gao WB. Six Consummate Skills of Acupuncturemoxibustion: Modern Acupuncture-moxibustion Therapies for Neuropathies. Beijing: Chinese Medical Science Press, 2012: 146–148.
Sun WP, Huang YN. Diagnosis of post-stroke deglutition disorders. Zhongguo Cuzhong Zazhi, 2007, 2(3): 226–230.
Kang LR, Zheng S. Effective acupoints of bulbar paralysis by professor Gao Weibin. Zhongguo Zhen Jiu, 2016, 36(4): 402–404.
Sauvé WM. Recognizing and treating pseudobulbar affect. CNS Spectr, 2016, 21(S1): 34–44.
Kubota T, Mishima H, Hanada M. Paralytic dysphagia in cerebrovascular disorder: screening tests and their clinical application. Sogo Rehabil, 1982, 10(4): 271–276.
Zhang CH, Bian JL, Meng ZH, Meng LN, Ren XS, Wang ZL, Guo XY, Shi XM. Tongguan Liqiao acupuncture therapy improves dysphagia after brainstem stroke. Neural Regen Res, 2016, 11(2): 285–291.
Wang GL. He Pu-ren and fire-needle therapy. Zhongguo Zhongyiyao Bao, 2016-09-08(4).
China Expert Consensus Group on Rehabilitation Evaluation and Treatment of Deglutition Disorders. China expert consensus on rehabilitation evaluation and treatment of deglutition disorders (2013). Zhonghua Wuli Yixue Yu Kangfu Zazhi, 2013, 35(12): 916–929.
Chan SL. Survey on acupuncture treatment of neurogenic dysphagia and analysis of regularity of acupoint selection. J Acupunct Tuina Sci, 2015, 13(5): 273–279.
Yu C, Shen B, Xu SW. Systematic review of acupuncturemoxibustion for deglutition disorders after cerebral stroke. Shanghai Zhenjiu Zazhi, 2016, 35(9): 1126–1129.
Chan SL. A Randomized Controlled Study on Therapeutic Effect of Acupuncture for Stroke Pseudobulbar Palsy Dysphagia. Nanjing: Doctor Thesis of Nanjing University of Chinese Medicine, 2017.
Chu JM, Liu XP, Chen FY, Hong FF, Bao YH. Effects of Gao’s neck acupuncture on swallowing function and quality of life in patients with post-stroke pseudobulbar palsy: a randomized controlled trial. Zhongguo Zhen Jiu, 2017, 37(7): 691–695.
Zhang YG. Clinical application study of acupuncture at glossopharyngeal acupoints for deglutition disorders due to pseudobulbar palsy after cerebral infarction. Zhongguo Xiandai Yaowu Yingyong, 2017, 11(24): 41–42.
Liu JY, Chen YH. Influence of acupoint-injection on TXB2 and 6-keto-PGF1a in patients with pseudobulbar palsy: a randomized controlled trial. J Acupunct Tuina Sci, 2017, 15(3): 22–26.
Su XQ. Randomised Controlled Trials of Pseudobulbar Palsy Dysphagia After Cerebral Infarction Treated by Acupuncture at the Tongue and Pharynx Acupoints. Harbin: Master Thesis of Heilongjiang University of Chinese Medicine, 2014.
Acknowledgments
This work was supported by National Natural Science Foundation of China (国家自然科学基金, No. 81473761, No. 81704181); Key Research Project of Economic and Social Development in Heilongjiang Province (黑龙江省 经济社会发展重点研究课题, No. JD2017019).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guo, Yh., Sun, Zr., Cai, S. et al. Fire-needle therapy for deglutition disorders in post-stroke pseudobulbar palsy: a randomized controlled trial. J. Acupunct. Tuina. Sci. 16, 375–381 (2018). https://doi.org/10.1007/s11726-018-1077-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11726-018-1077-4
Keywords
- Acupuncture Therapy
- Fire-needle Therapy
- Scalp Stimulation Areas
- Stroke
- Complications
- Pseudobulbar Palsy
- Deglutition Disorders
- Randomized Controlled Trials