Abstract
Objective
To observe the effect of balancing yin-yang needling manipulation on post-stroke upper limb spasticity and changes of electromyography (EMG) after treatment.
Methods
A total of 60 eligible cases were randomly allocated into an observation group and a control group, 30 in each group. Based on routine medication, cases in the control group were treated with conventional needling manipulation, whereas cases in the observation group were treated with balancing yin-yang manipulation. After the courses of treatment were completed, the therapeutic efficacies were evaluated using modified Ashworth scale and clinical spasticity index (CSI), coupled with the integrated electromyography (IEMG) and root mean square (RMS) value of biceps in passive flexion of the elbow joint during isokinetic testing recorded with the surface EMG.
Results
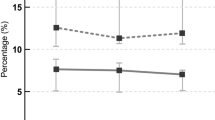
The total effective rate in the observation group was 86.7%, versus 53.3% in the control group, showing a statistical significance (P < 0.05). After treatment, there was between-group statistical significance in severity of elbow spasticity (P<0.05); there were intragroup (P<0.01, P<0.05) and inter-group (P<0.05) statistical significances in CSI index; and there were intra-group (P<0.01, P<0.05) and inter-group (P<0.01, P<0.05) statistical significances in IEMG and RMS values.
Conclusion
Balancing yin-yang and conventional needling manipulations can both improve upper limb spasm and reduce CSI as well as IEMG and RMS values in stroke patients; however, balancing yin-yang manipulation is better than conventional manipulation in clinical effect.
Similar content being viewed by others
References
Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379–380.
State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Beijing: China Medical Science Press, 2012: 186–187.
Shen XY. Meridians and Points. Beijing: China Press of Traditional Chinese Medicine, 2007: 44, 97, 162.
Blackburn M, van Vliet P, Mockett SP. Reliability of measurements obtained with the modified Ashworth scale in the lower extremities of people with stroke. Phys Ther, 2002, 82: 25–34.
Yan TB. Clinical spasticity index: clinical assessment index for spasticity. Xiandai Kangfu, 2000, 4(1): 88–89.
Bao ZZ, Li CL. Introduction to four-level weighted scoring for clinical diagnosis and efficacy evaluation. Zhongguo Linchuang Yaolixue Yu Zhiliaoxue, 2000, 5(2): 164–166.
Feldman RG, Young RR, Koella WP. Spasticity: Disordered Motor Control. Chicago: Year Book Medical Publishers, 1980: 485–494.
Young RR. Spasticity: a review. Neurology, 1994, 44(11 suppl 9): S12–S20.
Pandyan AD, Gregoric M, Barnes MP, Wood D, Van Wijck F, Burridge J, Hermens H, Johnson GR. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil, 2005, 27(1–2): 2–6.
Welmer AK, Widén Holmqvist L, Sommerfeld DK. Location and severity of spasticity in the first 1–2 weeks and at 3 and 18 months after stroke. Eur J Neurol, 2010, 17(5): 720–725.
Welmer AK, von Arbin M, Widén Holmqvist L, Sommerfeld DK. Spasticity and its association with functioning and health-related quality of life 18 months after stroke. Cerebrovasc Dis, 2006, 21(4): 247–253.
Kumar RT, Pandyan AD, Sharma AK. Biomechanical measurement of post-stroke spasticity. Age Ageing, 2006, 35(4): 371–375.
Wang YL. Evaluation on Rehabilitative Function. Beijing: People’s Medical Publishing House, 2008: 161.
Delisa JA, Nan DK, Guo ZC. Principle and Practice of Rehabilitation Medicine. 3rd Edition. Xi’an: World Publishing Xi’an Corporation Limited, 2004: 885–886.
Lundström E, Terént A, Borg J. Prevalence of disabling spasticity 1 year after first-ever stroke. Eur J Neurol, 2008, 15(6): 533–539.
Urban PP, Wolf T, Uebele M, Marx JJ, Vogt T, Stoeter P, Bauermann T, Weibrich C, Vucurevic GD, Schneider A, Wissel J. Occurence and clinical predictors of spasticity after ischemic stroke. Stroke, 2010, 41(9): 2016–2020.
Levin MF, Hui-Chan C. Ankle spasticity is inversely correlated with antagonist voluntary contraction in hemiparetic subjects. Electromyogr Clin Neurophysiol, 1994, 34(7): 415–425.
Levin MF, Hui-Chan C. Are H and stretch reflexes in hemiparesis reproducible and correlated with spasticity. J Neurol, 1993, 240(2): 63–71.
Zhao J, Li SR, Song WG. Pain Diagnosis and Management. Zhengzhou: Henan Medical University Press, 1999: 201–210.
Li ZL, Hua Y. Foundation of Chronic Pain Management. Beijing: People’s Military Medical Press, 2003: 27–38.
Lin CR, Zhang JX, Guo JK. Scalp acupuncture combined with Tianjing (TE 10) for elbow spasticity and paralysis following stroke in 15 cases. Liaoning Zhongyi Zazhi, 2010, 37(7): 1362–1364.
Shi XM. Acupuncture Therapeutics. Beijing: People’s Medical Publishing House, 2001: 212.
Niu WM, Li ZR. Study on mechanism of scalp electroacupuncture in treating ischemic stroke based on CT localization. J Acupunct Tuina Sci, 2006, 4(6): 333–335.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cui, Hf., Gao, Gq., Wang, Yl. et al. Therapeutic efficacy analysis of balancing yin-yang manipulation for post-stroke upper limb spasticity. J. Acupunct. Tuina. Sci. 12, 369–374 (2014). https://doi.org/10.1007/s11726-014-0808-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11726-014-0808-4