Abstract
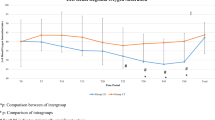
Little is known about the effects of CO2 insufflation (CDI) on cerebral oxygen saturation (CrSO2) during laparoscopy in the pediatric population. In children undergoing robotic-assisted laparoscopic pyeloplasty (RALP), we prospectively assessed the effects of CDI using standard monitoring and cerebral near-infrared spectroscopy (NIRS). We also explored whether a correlation existed between CrSO2 and parameters known to affect cerebral blood flow. Between January 2021 and September 2023, a cohort of consecutive children older than 2 years underwent RALP at Necker-Enfants Malades Hospital in Paris. A ventilation protocol aimed to prevent hypercarbia was implemented. Data collected included standard monitoring parameters and CrSO2 by NIRS. Thirty patients (16 females), mean age 5.5 ± 3.9 (2.0–9.5) years, were included. Twenty-three patients underwent a retroperitoneal approach. The mean baseline CrSO2 value was 83.0 ± 9.8. Mean CrSO2 decreased during progressive CDI, never below baseline values, while standard-monitoring parameters did not significantly change. No significant correlation was detected between CrSO2 and end tidal CO2, or between CrSO2 and mean arterial pressure, at any operative time. During RALP, a gradual CDI doesn’t cause pathological derangements of CrSO2. The lack of correlation between CrSO2 and standard parameters affecting cerebral blood flow suggests the likely presence of cerebral autoregulation in our population.
Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Lorenzo AJ, Karsli C, Halachmi S, Dolci M, Luginbuehl I, Bissonnette B, Farhat WA (2006) Hemodynamic and respiratory effects of pediatric urological retroperitoneal laparoscopic surgery: a prospective study. J Urol 175(4):1461–1465. https://doi.org/10.1016/S0022-5347(05)00668-3
Karsli C, El-Hout Y, Lorenzo AJ, Langer JC, Bägli DJ, Pippi Salle JL, Bissonette B, Farhat WA (2011) Physiological changes in transperitoneal versus retroperitoneal laparoscopy in children: a prospective analysis. J Urol 186:1649–1652. https://doi.org/10.1016/j.juro.2011.03.069
Pacilli M, Pierro A, Kingsley C, Curry JI, Herod J, Eaton S (2006) Absorption of carbon dioxide during laparoscopy in children measured using a novel mass spectrometric technique. Br J Anaesth 97:215–219. https://doi.org/10.1093/bja/ael134
McHoney M, Corizia L, Eaton S, Kiely EM, Drake DP, Tan HL, Spitz L, Pierro A (2003) Carbon dioxide elimination during laparoscopy in children is age dependent. J Pediatr Surg 38:105–110. https://doi.org/10.1053/jpsu.2003.50021
Cui B, Ou-Yang C, Xie S, Lin D, Ma J (2020) Age-related cerebrovascular carbon dioxide reactivity in children with ventricular septal defect younger than 3 years. Pediatr Anesth 30:977–983. https://doi.org/10.1111/pan.13967
Jildenstål P, Widarsson Norbeck D, Snygg J, Ricksten SE, Lannemyr L (2021) Cerebral autoregulation in infants during sevoflurane anesthesia for craniofacial surgery. Pediatr Anaesth 31:563–569. https://doi.org/10.1111/pan.14146
Weber F, Scoones GP (2019) A practical approach to cerebral near-infrared spectroscopy (NIRS) directed hemodynamic management in noncardiac pediatric anesthesia. Pediatr Anaesth 29:993–1001. https://doi.org/10.1111/pan.13726
Meng L, Gelb AW (2015) Regulation of cerebral autoregulation by carbon dioxide. Anesthesiology 122:196–205. https://doi.org/10.1097/ALN.0000000000000506
Franzini S, Querciagrossa S, Brebion M, Consonni D, Blanc T, Orliaguet G (2023) Effect of retropneumoperitoneum on cerebral and renal oxygen saturation during retroperitoneal robotic-assisted laparoscopic pyeloplasty (R-RALP) in a pediatric population: preliminary results of a prospective observational study using a dedicated anesthetic protocol and Near-Infrared spectroscopy. Anaesth Crit Care Pain Med 42:101234. https://doi.org/10.1016/j.accpm.2023.101234
Fleming S, Thompson M, Stevens R, Heneghan C, Plüddemann A, Maconochie I, Tarassenko L, Mant D (2011) Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet 377:1011–1018. https://doi.org/10.1016/S0140-6736(10)62226-X
Gómez-Pesquera E, Poves-Alvarez R, Martinez-Rafael B, Liu P, Alvarez J, Lorenzo-López M, Fierro I, Gómez-Sánchez E, Heredia-Rodriguez M, Gómez-Herreras JI, Tamayo E (2019) Cerebral oxygen saturation and negative postoperative behavioral changes in pediatric surgery: a prospective observational study. J Pediatr 208:207. https://doi.org/10.1016/j.jpeds.2018.12.047
Li L, Zhang J, Li J, Ren Y, Gao Z, Gao J, Zhang F, Wang F, Zheng T (2023) Development of a nomogram to predict negative postoperative behavioral changes based on a prospective cohort. BMC Anesthesiol 23:261. https://doi.org/10.1186/s12871-023-02228-4
Acknowledgements
The authors thank Sandra Colas and Sarah Bouchard (URC/CIC Necker Cochin, Paris, France) for their help in managing the protocol and collecting the data and Doctor Paolo Setti Carraro for writing assistance and for reviewing the manuscript. We would like to thank all staff from the Pediatric Anaesthesia Department and Pediatric Surgery Department at Hopital Universitaire Necker Enfants Malades for their support in this study.
Funding
The project was funded by a grant from Necker-Enfants Malades Hospital. The sponsor played no direct role in the study.
Author information
Authors and Affiliations
Contributions
SF, SQ, TB, GO: study design. SF, SQ, MB: data acquisition. SF, SQ, TB, GO: patient recruitment, data collection, analysis and interpretation of data. SF, GO, MB, TB, SQ, CL: writing of the first draft of the paper. All authors: article revision. All authors: final approval of the version of the manuscript to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
Thomas Blanc is an official proctor for Intuitive Surgical.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Franzini, S., Querciagrossa, S., Brebion, M. et al. Expanding safety boundaries in pediatric robotic-assisted laparoscopic surgery: are we protecting our children?. J Robotic Surg 18, 185 (2024). https://doi.org/10.1007/s11701-024-01959-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11701-024-01959-x