Abstract
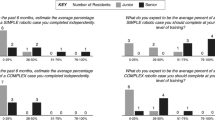
Trainee participation and progression in robotic general surgery remain poorly defined. Computer-assisted technology offers the potential to provide and track objective performance metrics. In this study, we aimed to validate the use of a novel metric—active control time (ACT)—for assessing trainee participation in robotic-assisted cases. Performance data from da Vinci Surgical Systems was retrospectively analyzed for all robotic cases involving trainees with a single minimally invasive surgeon over 10 months. The primary outcome metric was percent ACT—the amount of trainee console time spent in active system manipulations over total active time from both consoles. Kruskal–Wallis and Mann–Whitney U statistical tests were applied in analyses. A total of 123 robotic cases with 18 general surgery residents and 1 fellow were included. Of these, 56 were categorized as complex. Median %ACT was statistically different between trainee levels for all case types taken in aggregate (PGY1s 3.0% [IQR 2–14%], PGY3s 32% [IQR 27–66%], PGY4s 42% [IQR 26–52%], PGY5s 50% [IQR 28–70%], and fellow 61% [IQR 41–85%], p = < 0.0001). When stratified by complexity, median %ACT was higher in standard versus complex cases for PGY5 (60% vs. 36%, p = 0.0002) and fellow groups (74% vs. 47%, p = 0.0045). In this study, we demonstrated an increase in %ACT with trainee level and with standard versus complex robotic cases. These findings are consistent with hypotheses, providing validity evidence for ACT as an objective measurement of trainee participation in robotic-assisted cases. Future studies will aim to define task-specific ACT to guide further robotic training and performance assessments.



Similar content being viewed by others
Data Availability
The dataset generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2019.18911
Juo YY, Mantha A, Abiri A, Lin A, Dutson E (2018) Diffusion of robotic-assisted laparoscopic technology across specialties: a national study from 2008 to 2013. Surg Endosc 32:1405–1413
Mustafa S, Handren E, Farmer D, Ontiveros E, Ogola GO, Leeds SG (2019) Robotic curriculum enhances minimally invasive general surgery residents’ education. J Surg Educ 76:548–553
Winder JS, Juza RM, Sasaki J, Rogers AM, Pauli EM, Haluck RS, Estes SJ, Lyn-Sue JR (2016) Implementing a robotics curriculum at an academic general surgery training program: our initial experience. J Robot Surg 10:209–2013
Gerull W, Zihni A, Awad M (2020) Operative performance outcomes of a simulator-based robotic skills curriculum. Surg Endosc 34:4543–4548
Chen R, Rodrigues Armijo P, Krause C, Siu KC, Oleynikov D, SAGES Robotic Task Force (2020) A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg Endosc 34:361–367
Fernandes E, Elli E, Giulianotti P (2014) The role of the dual console in robotic surgical training. Surgery. https://doi.org/10.1016/j.surg.2013.06.023
Zhao B, Lam J, Hollandsworth HM, Lee AM, Lopez NE, Abbadessa B, Eisenstein S, Cosman BC, Ramamoorthy SL, Parry LA (2020) General surgery training in the era of robotic surgery: a qualitative analysis of perceptions from resident and attending surgeons. Surg Endosc 34:1712–1721
Mehaffey JH, Michaels AD, Mullen MG, Yount KW, Meneveau MO, Smith PW, Friel CM, Schirmer BD (2017) Adoption of robotics in a general surgery residency program: at what cost? J Surg Res. https://doi.org/10.1016/j.jss.2017.02.052
Khalafallah YM, Bernaiche T, Ranson S, Liu C, Collins DT, Dort J, Hafner G (2021) Residents’ views on the impact of robotic surgery on general surgery education. J Surg Educ 78:1007–1012
Shaw RD, Eid MA, Bleicher J, Broecker J, Caesar B, Chin R, Meyer C, Mitsakos A, Stolarksi AE, Theiss L, Smith BK, Ivatury SJ (2021) Current barriers in robotic surgery training for general surgery residents. J Surg Educ. https://doi.org/10.1016/j.jsurg.2021.11.005
Meyerson SL, Teitelbaum EN, George BC, Schuller MC, DaRosa DA, Fryer JP (2014) Defining the autonomy gap: when expectations do not meet reality in the operating room. J Surg Educ. https://doi.org/10.1016/j.jsurg.2014.05.002
Meyerson SL, Sternbach JM, Zwischenberger JB, Bender EM (2017) Resident autonomy in the operating room: expectations versus reality. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2017.05.034
Pernar LIM, Robertson FC, Tavakkoli A, Sheu EG, Brooks DC, Smink DS (2017) An appraisal of the learning curve in robotic general surgery. Surg Endosc. https://doi.org/10.1007/s00464-017-5520-2
Soomro NA, Hashimoto DA, Porteous AJ, Ridley CJA, Marsh WJ, Ditto R, Roy S (2020) Systematic review of learning curves in robot-assisted surgery. BJS Open. https://doi.org/10.1002/bjs5.50235
Hung AJ, Chen J, Gill IS (2018) Automated performance metrics and machine learning algorithms to measure surgeon performance and anticipate clinical outcomes in robotic surgery. JAMA Surg. https://doi.org/10.1001/jamasurg.2018.1512
Kumar R, Jog A, Vagvolgyi B, Nguyen H, Hager G, Chen CC, Yuh D (2012) Objective measures for longitudinal assessment of robotic surgery training. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2011.11.002
Chen J, Oh PJ, Cheng N, Shah A, Montez J, Jarc A, Guo L, Gill IS, Hung AJ (2018) Use of automated performance metrics to measure surgeon performance during robotic vesicourethral anastomosis and methodical development of a training tutorial. J Urol. https://doi.org/10.1016/j.juro.2018.05.080
Hung AJ, Chen J, Che Z, Nilanon T, Jarc A, Titus M, Oh PJ, Gill IS, Liu Y (2018) Utilizing machine learning and automated performance metrics to evaluate robot-assisted radical prostatectomy performance and predict outcomes. J Endourol. https://doi.org/10.1089/end.2018.0035
Kadakia N, Malek K, Lee SK, Lee EJ, Burruss S, Srikureja D, Mukherjee K, Lum SS (2020) Impact of robotic surgery on residency training for herniorrhaphy and cholecystectomy. Am Surg. https://doi.org/10.1177/0003134820964430
George BC, Bohnen JD, Williams RG, Meyerson SL, Schuller MC, Clark MJ, Meier AH, Torbeck L, Mandell SP, Mullen JT, Smink DS, Scully RE, Chipman JG, Auyang ED, Terhune KP, Wise PE, Choi JN, Foley EF, Dimick JB, Choti MA, Soper NJ, Lillemoe KD, Zwischenberger JB, Dunnington GL, DaRosa DA, Fryer JP, Procedural Learning and Safety Collaborative (PLSC) (2017) Readiness of US general surgery residents for independent practice. Ann Surg. https://doi.org/10.1097/SLA.0000000000002414
Booth KK, Stewart KE, Lewis SL, Garwe T, Kempenich JW, Lees JS (2021) Correlation of supervised independence and performance with procedure difficulty amongst surgical residents stratified by post graduate year. J Surg Educ. https://doi.org/10.1016/j.jsurg.2021.08.002
Gofton WT, Dudek NL, Wood TJ, Balaa F, Hamstra SJ (2012) The Ottawa surgical competency operating room evaluation (O-SCORE): a tool to assess surgical competence. Acad Med 87(10):1401–1407
Bohnen JD, George BC, Williams RG, Schuller MC, DaRosa DA, Torbeck L, Mullen JT, Meyerson SL, Auyang ED, Chipman JG, Choi JN, Choti MA, Endean ED, Foley EF, Mandell SP, Meier AH, Smink DS, Terhune KP, Wise PE, Soper NJ, Zwischenberger JB, Lillemoe KD, Dunnington GL, Fryer JP, Procedural Learning and Safety Collaborative (PLSC) (2016) The feasibility of real-time intraoperative performance assessment with SIMPL (system for improving and measuring procedural learning): early experience from a multi-institutional trial. J Surg Educ 73(6):118–130
Eaton M, Scully R, Schuller M, Yang A, Smink D, Williams RG, Bohnen JD, George BC, Fryer JP, Meyerson SL (2019) Value and barriers to use of the SIMPL tool for resident feedback. J Surg Educ. https://doi.org/10.1016/j.jsurg.2019.01.012
Sánchez R, Rodríguez O, Rosciano J, Vegas L, Bond V, Rojas A, Sanchez-Ismayel A (2016) Robotic surgery training: construct validity of global evaluative assessment of robotic skills (GEARS). J Robot Surg. https://doi.org/10.1007/s11701-016-0572-1
Liu M, Purohit S, Mazanetz J, Allen W, Kreaden US, Curet M (2018) Assessment of Robotic Console Skills (ARCS): construct validity of a novel global rating scale for technical skills in robotically assisted surgery. Surg Endosc. https://doi.org/10.1007/s00464-017-5694-7
Intuitive Surgical, Inc. 2021 Annual Report. https://www.annualreports.com/HostedData/AnnualReports/PDF/NASDAQ_ISRG_2021.pdf. Accessed 25 Mar 2022
Tousignant MR, Liu X, Ershad Langroodi M, Jarc AM (2022) Identification of main influencers of surgical efficiency and variability using task-level objective metrics: a five-year robotic sleeve gastrectomy case series. Front Surg. https://doi.org/10.3389/fsurg.2022.756522
Zia A, Zhang C, Xiong X, Jarc AM (2017) Temporal clustering of surgical activities in robot-assisted surgery. Int J Comput Assist Radiol Surg. https://doi.org/10.1007/s11548-017-1600-y
Acknowledgements
The authors thank Sylvia Padilla for her assistance with organization of performance metric data obtained from the da Vinci Surgical System.
Funding
The authors declare that no funds, grants, or other support were received during the study or preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Author MMA conceived and designed the study. Authors JMC and AY performed data collection, assembly, analysis, and interpretation. All authors contributed to manuscript writing and final approvals.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Awad has educational grants from Applied Medical, Bard/BD Medical, Baxter, Ethicon, Medtronic, and Stryker for simulation training. He is also a consultant for Ethicon, Intuitive Surgical, and Medtronic. Dr. Yee had no conflicts during this study, however, has become an employee of Intuitive Surgical after its completion. Dr. Clanahan has no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clanahan, J.M., Yee, A. & Awad, M.M. Active control time: an objective performance metric for trainee participation in robotic surgery. J Robotic Surg 17, 2117–2123 (2023). https://doi.org/10.1007/s11701-023-01628-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-023-01628-5