Abstract
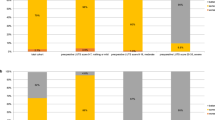
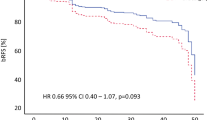
The objective is to evaluate the effect of robot-assisted radical prostatectomy (RARP)-related postoperative complications on the 6-month postoperative health-related quality of life (HRQoL). A total of 1008 patients underwent a RARP with or without pelvic lymph node dissection (PLND) between 2012 and 2020 and were invited to complete questionnaires about HRQoL and functional outcomes (urinary incontinence (UI), erectile dysfunction (ED) and urinary complaints (UC)) before and 6 months after RARP. Patient characteristics and postoperative complications up to 90 days after surgery were prospectively recorded. Associations between complications and HRQoL/functional outcomes were assessed by multivariate linear regression analyses. In total, 528 patients (52.4%) were included in the analyses. Complications occurred in 165/528 (31.3%) patients, of which 30/165 (18.2%) had a Clavien–Dindo ≥ III complication. In multivariate regression analyses, postoperative complications were not significantly associated with postoperative HRQoL, UI and ED (p = 0.73, p = 0.72 and p = 0.95, respectively), but were significantly associated with a minor increase in UC (β = 1.7, p < 0.001). More specifically, infectious and urological complications were significantly associated with an increase in UC (β = 1.9, p < 0.001 and β = 0.9, p = 0.004, respectively). The presence of UTI, in particular, was significantly associated with this minor increase (β = 1.5, p = 0.002). Functional outcomes were all significantly associated with the HRQoL at 6 months postoperatively. No significant associations were found between postoperative complications and HRQoL at 6 months after RARP. However, worse functional outcomes were associated with a worse HRQoL at 6 months postoperatively. In addition, postoperative infectious and urological complications were significantly associated with a minor increase in UC.

Similar content being viewed by others
Availability of data and material
Available upon request.
Code availability
Not applicable.
References
Shao I-H, Chang Y-H, Hou C-M, Lin Z-F, Wu C-T (2017) Predictors of short-term and long-term incontinence after robot-assisted radical prostatectomy. J Int Med Res 46(1):421–429. https://doi.org/10.1177/0300060517715396
Dagrosa LM, Ingimarsson JP, Gorlov IP, Higgins JH, Hyams ES (2016) Is age an independent risk factor for medical complications following minimally invasive radical prostatectomy? An evaluation of contemporary American College of Surgeons National Surgical Quality Improvement (ACS-NSQIP) data. J Robot Surg 10(4):343–346. https://doi.org/10.1007/s11701-016-0605-9
Porcaro AB, Sebben M, Tafuri A, de Luyk N, Corsi P, Processali T, Pirozzi M, Rizzetto R, Amigoni N, Mattevi D, Cerruto MA, Brunelli M, Novella G, De Marco V, Migliorini F, Artibani W (2018) Body mass index is an independent predictor of Clavien–Dindo grade 3 complications in patients undergoing robot assisted radical prostatectomy with extensive pelvic lymph node dissection. J Robot Surg 13(1):83–89. https://doi.org/10.1007/s11701-018-0824-3
Babaian KN, Skarecky D, Liss MA, Osann K, Lusch A, Ahlering TE (2014) A comparative analysis of complications after robot-assisted radical prostatectomy for men aged ≤69 and ≥70 years. J Endourol 28(12):1435–1438. https://doi.org/10.1089/end.2014.0234
Vernooij RWM, Cremers RGHM, Jansen H, Somford DM, Kiemeney LA, van Andel G, Wijsman BP, Busstra MB, van Moorselaar RJA, Wijnen EM, Pos FJ, Hulshof MCCM, Hamberg P, van den Berkmortel F, Hulsbergen-van de Kaa CA, van Leenders GJLH, Fütterer JJ, van Oort IM, Aben KKH (2020) Urinary incontinence and erectile dysfunction in patients with localized or locally advanced prostate cancer: a nationwide observational study. Urol Oncol 38(9):735–735. https://doi.org/10.1016/j.urolonc.2020.05.022
Dąbrowska-Bender M, Słoniewski R, Religioni U, Juszczyk G, Słoniewska A, Staniszewska A (2017) Analysis of quality of life subjective perception by patients treated for prostate cancer with the EORTC QLQ-C30 QUestionnaire and QLQ-PR25 Module. J Cancer Educ 32(3):509–515. https://doi.org/10.1007/s13187-015-0954-5
Terrier JE, Mulhall JP, Nelson CJ (2017) Exploring the optimal erectile function domain score cutoff that defines sexual satisfaction after radical prostatectomy. J Sex Med 14(6):804–809. https://doi.org/10.1016/j.jsxm.2017.04.672
Gardner TA, Bissonette EA, Petroni GR, McClain R, Sokoloff MH, Theodorescu D (2000) Surgical and postoperative factors affecting length of hospital stay after radical prostatectomy. Cancer 89(2):424–430. https://doi.org/10.1002/1097-0142(20000715)
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA (2015) The 2014 International Society of Urological Pathology (ISUP) Consensus conference on Gleason grading of prostatic carcinoma. Am J Surg Pathol. https://doi.org/10.1097/pas.0000000000000530
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, Haes JCJM, Kaasa S, Klee M, Osoba D, Razavi D, Rofe PB, Schraub S, Sneeuw K, Sullivan M, Takeda F (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. JNCI 85(5):365–376. https://doi.org/10.1093/jnci/85.5.365
van Andel G, Bottomley A, Fosså SD, Efficace F, Coens C, Guerif S, Kynaston H, Gontero P, Thalmann G, Akdas A, D’Haese S, Aaronson NK (2008) An international field study of the EORTC QLQ-PR25: a questionnaire for assessing the health-related quality of life of patients with prostate cancer. Eur J Cancer 44(16):2418–2424. https://doi.org/10.1016/j.ejca.2008.07.030
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49(6):822–830. https://doi.org/10.1016/s0090-4295(97)00238-0
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P (2004) ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn 23(4):322–330. https://doi.org/10.1002/nau.20041
Badia X, Garcia-Losa M, Dal-Ré R (1997) Ten-language translation and harmonization of the international prostate symptom score: developing a methodology for multinational clinical trials. Eur Urol 31(2):129–140. https://doi.org/10.1159/000474438
van der Poel HG, de Blok W (2009) Role of extent of fascia preservation and erectile function after robot-assisted laparoscopic prostatectomy. Urology 73(4):816–821. https://doi.org/10.1016/j.urology.2008.09.082
Briganti A, Larcher A, Abdollah F, Capitanio U, Gallina A, Suardi N, Bianchi M, Sun M, Freschi M, Salonia A, Karakiewicz PI, Rigatti P, Montorsi F (2012) Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol 61(3):480–487. https://doi.org/10.1016/j.eururo.2011.10.044
Husson O, Rooij BH, Kieffer J, Oerlemans S, Mols F, Aaronson NK, Graaf WTA, Poll-Franse LV (2019) The EORTC QLQ-C30 summary score as prognostic factor for survival of patients with cancer in the “Real-World”: results from the population-based PROFILES Registry. Oncologist 25(4):e722–e732. https://doi.org/10.1634/theoncologist.2019-0348
Löppenberg B, von Bodman C, Brock M, Roghmann F, Noldus J, Palisaar RJ (2014) Effect of perioperative complications and functional outcomes on health-related quality of life after radical prostatectomy. Qual Life Res 23(10):2743–2756. https://doi.org/10.1007/s11136-014-0729-1
Sprangers MAG, Schwartz CE (1999) The challenge of response shift for quality-of-life-based clinical oncology research. Ann Oncol 10(7):747–749. https://doi.org/10.1023/a:10083055235
Wallerstedt A, Nyberg T, Carlsson S, Thorsteinsdottir T, Stranne J, Tyritzis SI, Stinesen Kollberg K, Hugosson J, Bjartell A, Wilderäng U, Wiklund P, Steineck G, Haglind E (2019) Quality of life after open radical prostatectomy compared with robot-assisted radical prostatectomy. Eur Urol Focus 5(3):389–398. https://doi.org/10.1016/j.euf.2017.12.010
Miyake H, Miyazaki A, Furukawa J, Hinata N, Fujisawa M (2016) Prospective assessment of time-dependent changes in quality of life of Japanese patients with prostate cancer following robot-assisted radical prostatectomy. J Robot Surg 10(3):201–207. https://doi.org/10.1007/s11701-016-0565-0
Ngoo KS, Honda M, Kimura Y, Yumioka T, Iwamoto H, Morizane S, Hikita K, Takenaka A (2019) Longitudinal study on the impact of urinary continence and sexual function on health-related quality of life among Japanese men after robot-assisted radical prostatectomy. Int J Med Robot Comput Assist Surg 15(4):e2018. https://doi.org/10.1002/rcs.2018
van der Poel HG, Tillier C, de Blok WM, Acar C, van Muilekom EH, van den Bergh RC (2013) Interview-based versus questionnaire-based quality of life outcomes before and after prostatectomy. J Endourol 27(11):1411–1416. https://doi.org/10.1089/end.2012.0735
Bayoud Y, de la Taille A, Ouzzane A, Ploussard G, Allory Y, Yiou R, Vordos D, Hoznek A, Salomon L (2015) International Prostate Symptom Score is a predictive factor of lower urinary tract symptoms after radical prostatectomy. Int J Urol 22(3):283–287. https://doi.org/10.1111/iju.12681
Funding
No funding was obtained.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hagens, M.J., Veerman, H., de Ligt, K.M. et al. Functional outcomes rather than complications predict poor health-related quality of life at 6 months after robot-assisted radical prostatectomy. J Robotic Surg 16, 453–462 (2022). https://doi.org/10.1007/s11701-021-01266-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-021-01266-9