Abstract
Introduction
One Anastomosis Duodenal Switch (OADS/SADI-S) is used both as a one stage and a second-step procedure, either planned or revisional after a failed sleeve gastrectomy. However, there is lack of adjusted comparative evidence validating its use.
Material and Methods
Propensity-score matched comparison between patients submitted to one-stage vs. two-step OADS, adjusted by age, gender, and initial body mass index (BMI).
Results
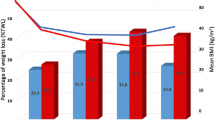
One hundred ninety-five patients (130 one-stage and 65 two-step OADS) were included, with mean initial BMI 52.4 kg/m2. Overall complication rate was 6.6% in the short-term (3.3% Clavien-Dindo ≥ III), and 7.3% in the long-term, with no differences between groups. Follow-up at 1 and 3 years was 83.6% and 61.5%. After one-stage OADS, total weight loss was 36.6 ± 8.2% at 1 year and 30.4 ± 10.3% at 3 years, vs. 30.2 ± 9.4% and 25.6 ± 10.2% after two-steps OADS (p = 0.021). Resolution rates of diabetes mellitus, hypertension, dyslipidemia, and obstructive sleep apnea were 86.4%, 80.4%, 78.0%, and 73.3%, with no differences between groups.
Conclusion
One-stage OADS is a safe and effective bariatric technique for patients with grade III and IV obesity. The two-step strategy does not reduce postoperative risks and may compromise weight loss results at mid-term.
Graphical Abstract




Similar content being viewed by others
References
Hess DS, Hess DW, Oakley RS. The biliopancreatic diversion with the duodenal switch: results beyond 10 years. Obes Surg. 2005;15(3):408–16.
Risstad H, Søvik TT, Engström M, et al. Five-year outcomes after laparoscopic gastric bypass and laparoscopic duodenal switch in patients with body mass index of 50 to 60: a randomized clinical trial. JAMA Surg. 2015;150(4):352–61.
Strain GW, Torghabeh MH, Gagner M, et al. The impact of biliopancreatic diversion with duodenal switch (BPD/DS) over 9 years. Obes Surg. 2017;27(3):787–94.
Maroun J, Li M, Oyefule O, et al. Ten year comparative analysis of sleeve gastrectomy, Roux-en-Y gastric bypass, and biliopancreatic diversion with duodenal switch in patients with BMI ≥ 50 kg/m2. Surg Endosc. 2022;36(7):4946–55.
Angrisani L, Santonicola A, Iovino P, et al. IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28(12):3783–94.
Clapp B, Badaoui JN, Gamez JA, et al. Reluctance in duodenal switch adoption: an international survey among bariatric surgeons. Surg Obes Relat Dis. 2021;17(10):1760–5.
Dapri G, Cadière GB, Himpens J. Superobese and super-superobese patients: 2-step laparoscopic duodenal switch. Surg Obes Relat Dis. 2011;7(6):703–8.
Topart P, Becouarn G, Ritz P. Should biliopancreatic diversion with duodenal switch be done as single-stage procedure in patients with BMI > or = 50 kg/m2? Surg Obes Relat Dis. 2010;6(1):59–63.
Iannelli A, Schneck AS, Topart P, et al. Laparoscopic sleeve gastrectomy followed by duodenal switch in selected patients versus single-stage duodenal switch for superobesity: case-control study. Surg Obes Relat Dis. 2013;9(4):531–8.
Gagner M, Hutchinson C, Rosenthal R. Fifth International Consensus Conference: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(4):750–6.
Lee Y, Ellenbogen Y, Doumouras AG, et al. Single- or double-anastomosis duodenal switch versus Roux-en-Y gastric bypass as a revisional procedure for sleeve gastrectomy: a systematic review and meta-analysis. Surg Obes Relat Dis. 2019;15(4):556–66.
Osorio J, Lazzara C, Admella V, et al. Revisional Laparoscopic SADI-S vs. Duodenal switch following failed primary sleeve gastrectomy: a single-center comparison of 101 consecutive cases. Obes Surg. 2021;31(8):3667–74.
Sánchez-Pernaute A, Herrera MA, Pérez-Aguirre ME, et al. Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up. Obes Surg. 2010;20(12):1720–6.
Sánchez-Pernaute A, Herrera MÁR, Ferré NP, et al. Long-term results of single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). Obes Surg. 2022;32(3):682–9.
Finno P, Osorio J, García-Ruiz-de-Gordejuela A, et al. Single versus double-anastomosis duodenal switch: single-site comparative cohort study in 440 consecutive patients. Obes Surg. 2020;30(9):3309–16.
Gebellí JP, Lazzara C, de Gordejuela AGR, et al. Duodenal switch vs. single-anastomosis duodenal switch (SADI-S) for the treatment of grade IV obesity: 5-year outcomes of a multicenter prospective cohort comparative study. Obes Surg. 2022;32(12):3839–46.
Surve A, Cottam D, Medlin W, et al. Long-term outcomes of primary single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). Surg Obes Relat Dis. 2020;16(11):1638–46.
Sánchez-Pernaute A, Rubio MÁ, Pérez N, et al. Single-anastomosis duodenoileal bypass as a revisional or second-step operation after sleeve gastrectomy. Surg Obes Relat Dis. 2020;16(10):1491–6.
Balibrea JM, Vilallonga R, Hidalgo M, et al. Mid-term results and responsiveness predictors after two-step single-anastomosis duodeno-ileal bypass with sleeve gastrectomy. Obes Surg. 2017;27(5):1302–8.
Barajas-Gamboa JS, Moon S, Romero-Velez G, et al. Primary single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) versus sleeve gastrectomy to SADI conversions: a comparison study of prevalence and safety. Surg Endosc. 2023;37(11):8682–9.
Verhoeff K, Mocanu V, Jogiat U, et al. Patient selection and 30-day outcomes of SADI-S compared to RYGB: a retrospective cohort study of 47,375 patients. Obes Surg. 2022;32(7):1–8.
Gebelli JP, Gordejuela AG, Ramos AC, et al. SADI-S with right gastric artery ligation: technical systematization and early results. Arq Bras Cir Dig. 2016;29Suppl 1(Suppl 1):85–90.
Biertho L, Simon-Hould F, Marceau S, et al. Current outcomes of laparoscopic duodenal switch. Ann Surg Innov Res. 2016;10:1.
- Summerhays C, Cottam D, Cottam A. Internal hernia after revisional laparoscopic loop duodenal switch surgery. Surg Obes Relat Dis. Elsevier Inc. 2016;12:e13–5.
Sethi M, Chau E, Youn A, et al. Long-term outcomes after biliopancreatic diversion with and without duodenal switch: 2-,5-, and 10-year data. Surg Obes Relat Dis. 2016;12:1697–705.
Bruzzi M, Rau C, Voron T, et al. Single anastomosis or minigastric bypass: longterm results and quality of life after a 5 year followup. Surg Obes Relat Dis. 2015;11:321–6.
Rutledge R, Kular K, Manchanda N. The minigastric bypass original technique. Int J Surg. 2019;61:38–41.
Sitarz R, Maciejewski R, Polkowski WP, et al. Gastroenterostoma after Billroth antrectomy as a premalignant condition. World J Gastroenterol. 2012;18:3201–6.
Verhoeff K, Mocanu V, Zalasky A, et al. Evaluation of metabolic outcomes following SADI-S: a systematic review and meta-analysis. Obes Surg. 2022;32(4):1049–63.
Palermo M, Acquafresca PA, Rogula T, et al. Late surgical complications after gastric by-pass: a literature review. Arq Bras Cir Dig. 2015;28(2):139–43.
Poljo A, Pentsch A, Raab S, et al. Incidence of dumping syndrome after sleeve gastrectomy, Roux-en-y gastric bypass and one-anastomosis gastric bypass. J Metab Bariatr Surg. 2021;10(1):23–31.
Pereira AM, Guimarães M, Pereira SS, et al. Single and dual anastomosis duodenal switch for obesity treatment: a single-center experience. Surg Obes Relat Dis. 2021;17(1):12–9.
Shoar S, Poliakin L, Rubenstein R, et al. Single anastomosis duodeno-ileal switch (SADIS): a systematic review of efficacy and safety. Obes Surg. 2018;28(1):104–13.
Skogar ML, Sundbom M. Duodenal switch is superior to gastric bypass in patients with super obesity when evaluated with the bariatric analysis and reporting outcome system (BAROS). Obes Surg. 2017;27(9):2308–16.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Hedberg J, Sundström J, Sundbom M. Duodenal switch versus Roux-en-Y gastric bypass for morbid obesity: systematic review and meta-analysis of weight results, diabetes resolution and early complications in single-centre comparisons. Obes Rev. 2014;15(7):555–63.
Sucandy I, Titano J, Bonanni F, et al. Comparison of vertical sleeve gastrectomy versus biliopancreatic diversion. N Am J Med Sci. 2014;6(1):35–8.
Prachand VN, Davee RT, Alverdy JC. Duodenal switch provides superior weight loss in the super-obese (BMI > or =50 kg/m2) compared with gastric bypass. Ann Surg. 2006;244(4):611–9.
Admella V, Osorio J, Sorribas M, et al. Direct and two-step single anastomosis duodenal switch (SADI-S): unicentric comparative analysis of 232 cases. Cir Esp (Engl Ed). 2021;99(7):514–20.
Pereira SS, Guimarães M, Almeida R, et al. Biliopancreatic diversion with duodenal switch (BPD-DS) and single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) result in distinct post-prandial hormone profiles. Int J Obes (Lond). 2019;43(12):2518–27.
Acknowledgements
The authors would like to thank Esther García Lerma and Natàlia Pallarès Fontanet, specialists in biostatistics, for their essential help in this study’s design and analysis. We would also like to thank Fernando Guerrero, endocrinologist, and the rest of the severe obesity treatment multidisciplinary team in Bellvitge University Hospital, for their contribution in the study, treatment, and follow-up of all patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• One-stage OADS is a safe and effective bariatric technique.
• Two-step OADS does not reduce postoperative risks in comparison to one-stage OADS.
• Two-step OADS may compromise weight loss results at mid-term.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Osorio, J., Admella, V., Merino, D. et al. One-Stage Vs. Two-Step One Anastomosis Duodenal Switch (OADS/SADI-S): A Safety and Efficacy Single-Center Propensity-Score Matched Analysis. OBES SURG (2024). https://doi.org/10.1007/s11695-024-07280-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11695-024-07280-8