Abstract
Background
Less than 50% of eligible candidates who are referred complete Bariatric Metabolic Surgery (BMS). The factors influencing the decision to complete BMS, particularly how these factors vary across different racial and ethnic groups, remain largely unexplored.
Methods
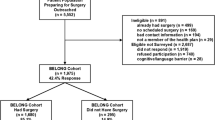
This prospective cohort study included adult patients referred to a bariatric surgeon or obesity medicine program between July 2019-September 2022. Sociodemographic characteristics, body mass index (BMI), anxiety, depression, body appreciation, and patient-physician relationship information were collected via survey and electronic health records. The association between BMS completion and potential decision-driving factors was examined using Classification and Regression Tree (CART) analysis.
Results
A total of 406 BMS -eligible patients participated in the study (mean [SD] age: 47.5 [11.6] years; 87.2% women; 18.0% Hispanic, 39% non-Hispanic Black [NHB], and 39% non-Hispanic White [NHW]; mean [SD] BMI: 45.9 [10.1] kg/m2). A total of 147 participants (36.2%) completed BMS. Overall, the most influential factor driving the decision to complete BMS was younger age (< 68.4 years), higher patient satisfaction, and BMI (≥ 38.0 kg/m2). Hispanic participants prioritized age (< 55.4 years), female sex, and body appreciation. For NHB participants, the highest ranked factors were age < 56.3 years, BMI ≥ 35.8 kg/m2, and higher patient satisfaction. For NHW patients, the most influential factors were age (39.1 to 68.6 years) and higher body appreciation.
Conclusion
These findings highlight racial and ethnic group differences in the factors motivating individuals to complete BMS. By acknowledging these differences, healthcare providers can support patients from different backgrounds more effectively in their decision-making process regarding BMS.
Graphical abstract




Similar content being viewed by others
Data Availability
Drs. Xie and Messiah had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013 [published correction appears in Lancet. Lancet. 2014;384(9945):766–781. https://doi.org/10.1016/S0140-6736(14)60460-8.
Puzziferri N, Roshek TB 3rd, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014;312(9):934–42. https://doi.org/10.1001/jama.2014.10706.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric Surgery Worldwide 2013. Obes Surg. 2015;25(10):1822–32. https://doi.org/10.1007/s11695-015-1657-z.
Jakobsen GS, Småstuen MC, Sandbu R, et al. Association of Bariatric Surgery vs Medical Obesity Treatment With Long-term Medical Complications and Obesity-Related Comorbidities. JAMA. 2018;319(3):291–301. https://doi.org/10.1001/jama.2017.21055.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89. https://doi.org/10.1007/s11695-011-0472-4.
Sarwer DB, Wadden TA, Moore RH, et al. Preoperative eating behavior, postoperative dietary adherence, and weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2008;4(5):640–6. https://doi.org/10.1016/j.soard.2008.04.013.
Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning: Data Mining, Inference, and Prediction. 2009. Springer-Verlag.
Ngenge S, Xie L, McAdams C, et al. Depression and Anxiety as Predictors of Metabolic and Bariatric Surgery Completion Among Ethnically Diverse Patients. Obes Surg. 2023;33(7):2166–75. https://doi.org/10.1007/s11695-023-06652-w.
Kapera O, Xie L, Marroquín EM, et al. The Role of Body Appreciation in the Decision to Complete Metabolic and Bariatric Surgery Among Ethnically Diverse Patients. Obes Surg. 2023;33(3):879–89. https://doi.org/10.1007/s11695-023-06456-y.
Xie L, Almandoz JP, Mathew MS, et al. Association Between Patient Satisfaction With Their Patient-Physician Relationship and Completion of Bariatric Surgery by Race and Ethnicity Among US Adults. JAMA Netw Open. 2022;5(12):e2247431. Published 2022 Dec 1. https://doi.org/10.1001/jamanetworkopen.2022.47431.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33.
Avalos L, Tylka TL, Wood-Barcalow N. The body appreciation scale: development and psychometric evaluation. Body Image. 2005;2(3):285–97.
Marshall GN, Hays RD. The Patient Satisfaction Questionnaire Short-Form (PSQ-18). RAND; 1994.
Loh WY. Classification and regression trees. Wiley interdisciplinary reviews: data mining and knowledge discovery. 2011;1(1):14–23. https://doi.org/10.1002/widm.8.
Breiman L, Friedman JH, Olshen RA, et al. Classification and regression trees. Routledge; 2017.
Gonzalez-Heredia R, Patel N, Sanchez-Johnsen L, et al. Does Age Influence Bariatric Surgery Outcomes? Bariatr Surg Pract Patient Care. 2015;10(2):74–8. https://doi.org/10.1089/bari.2015.0004.
Davidson LE, Adams TD, Kim J, et al. Association of Patient Age at Gastric Bypass Surgery With Long-term All-Cause and Cause-Specific Mortality. JAMA Surg. 2016;151(7):631–7. https://doi.org/10.1001/jamasurg.2015.5501.
Stokes A, Collins JM, Grant BF, et al. Prevalence and Determinants of Engagement with Obesity Care in the United States. Obesity (Silver Spring). 2018;26(5):814–8. https://doi.org/10.1002/oby.22173.
Axelrod DA, Goold SD. Maintaining trust in the surgeon-patient relationship: challenges for the new millennium. Arch Surg. 2000;135(1):55–61.
Williams S, Weinman J, Dale J. Doctor-patient communication and patient satisfaction: a review. Fam Pract. 1998;15(5):480–92.
Ghosh A, Sharma K, Choudhury S. COVID-19 and physician-patient relationship: potential effects of “masking”, “distancing” and “others”. Fam Pract. 2021;38(2):193–4.
Lee YC, Wu WL. Shared decision making and choice for bariatric surgery. Int J Environ Res Public Health. 2019;16(24):4966.
DeJesus RS, Bauer KW, Bradley DP, et al. Experience and expectations of patients on weight loss: The Learning Health System Network Experience. Obes Sci Pract. 2019;5(5):479–486. Published 2019 Aug 22. https://doi.org/10.1002/osp4.364.
Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5(7):161. https://doi.org/10.21037/atm.2017.03.107.
Richardson A, Allen JA, Xiao H, et al. Effects of race/ethnicity and socioeconomic status on health information-seeking, confidence, and trust. J Health Care Poor Underserved. 2012;23(4):1477–93. https://doi.org/10.1353/hpu.2012.0181.
Larkey LK, Hecht ML, Miller K, et al. Hispanic cultural norms for health-seeking behaviors in the face of symptoms. Health Educ Behav. 2001;28(1):65–80. https://doi.org/10.1177/109019810102800107.
Eley NT, Namey E, McKenna K, et al. Beyond the Individual: Social and Cultural Influences on the Health-Seeking Behaviors of African American Men. Am J Mens Health. 2019;13(1):1557988319829953. https://doi.org/10.1177/1557988319829953.
Hewins-Maroney B, Schumaker A, Williams E. Health seeking behaviors of African Americans: implications for health administration. J Health Hum Serv Adm. 2005;28(1):68–95.
Hosseini SA, Padhy RK. Body Image Distortion. [Updated 2023 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546582/. Accessed 15 Dec 2023.
Webb J. B. Acceptance and commitment therapy to facilitate positive body image and embodiment. In T. L. Tylka & N. Piran (Eds.), Handbook of positive body image and embodiment: Constructs, protective factors, and interventions (pp 288–299). 2009. Oxford University Press. https://doi.org/10.1093/med-psych/9780190841874.003.0028.
Manuel JI. Racial/Ethnic and Gender Disparities in Health Care Use and Access. Health Serv Res. 2018;53(3):1407–29. https://doi.org/10.1111/1475-6773.12705.
Paz K, Massey KP. Health Disparity among Latina Women: Comparison with Non-Latina Women. Clin Med Insights Womens Health. 2016;9(Suppl 1):71–74. Published 2016 Jul 20. https://doi.org/10.4137/CMWH.S38488.
Funding
This work was funded by the National Institutes of Health, National Institute on Minority Health and Health Disparities (Grants R01MD011686).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Role of the Funder
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
No conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• In the overall study population, the most influential factors driving the decision to complete Bariatric Metabolic Surgery (BMS) include younger age, higher patient satisfaction, and higher body mass index.
• There are racial and ethnic group differences in the factors motivating individuals to complete BMS.
• There is a need for future studies that aim to develop effective interventions to support decision-making for BMS among patients from diverse backgrounds.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xie, L., Atem, F., Mathew, M.S. et al. Factors Associated with the Decision to Complete Bariatric Metabolic Surgery among a Racially and Ethnically Diverse Sample of Adults: A Classification and Regression Tree Analysis. OBES SURG 34, 1513–1522 (2024). https://doi.org/10.1007/s11695-023-06999-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06999-0