Abstract
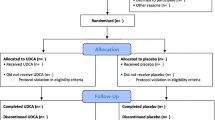
The aim of this meta-analysis was to assess whether treatment with ursodeoxycholic acid (UDCA) in patients who have undergone bariatric surgery reduces gallstone formation. A systematic literature search was performed using electronic databases (MEDLINE, Embase, CENTRAL, Web of Science, PROSPERO, Google Scholar and the WHO International Clinical Trials Registry platform). RCTs without restrictions on study language, year, status of publication and patient’s age were used. Pooled risk ratios were calculated using a random-effects model. Subgroup analyses for drug dose, duration and procedure types were performed. Sensitivity analyses and a summary of findings table were generated to assess the robustness and the level of evidence provided, respectively. Fourteen trials were included (3619 patients, 2292 in UDCA vs 1327 in control group). Procedures included SG, RYGB, OAGB, AGB and Gastroplasty. UDCA dose ranged from 300 to 1200 mg per day. Gallstone formation occurred in 19.3% (8.3% in UDCA vs 38.1% in the control group). UDCA significantly reduced the risk of gallstone formation (14 trials, 3619 patients; RR 0.27, 95% CI 0.18–0.41; P < 0.001). UDCA significantly reduced the risk of symptomatic gallstone disease (6 trials, 2458 patients; RR 0.30, 95% CI 0.21–0.43; P < 0.001). No subgroup difference was found for different doses, duration and type of procedure performed. Oral UDCA treatment significantly reduces the risks of developing gallstones in postoperative bariatric patients from 38 to 8%. The use of 500 to 600 mg UDCA for 6 months is effective and should be implemented in all patients post-bariatric surgery.
Graphical Abstract






Similar content being viewed by others
Data Availability
The authors declare that all relevant data used to conduct this review are included in the manuscript and supplements. Data is available from the corresponding author upon reasonable request.
References
NHS I. Statistics on obesity, physical activity and diet. England; 2011. 2019.
Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ : British Medical Journal. 2013;347:f5934.
Desbeaux A, Hec F, Andrieux S, et al. Risk of biliary complications in bariatric surgery. J Visc Surg. 2010;147(4):e217–20.
Gustafsson U, Benthin L, Granström L, et al. Changes in gallbladder bile composition and crystal detection time in morbidly obese subjects after bariatric surgery. Hepatology. 2005;41(6):1322–8.
Gebhard RL, Prigge WF, Ansel HJ, et al. The role of gallbladder emptying in gallstone formation during diet-induced rapid weight loss. Hepatology. 1996;24(3):544–8.
Manatsathit W, Leelasinjaroen P, Al-Hamid H, et al. The incidence of cholelithiasis after sleeve gastrectomy and its association with weight loss: a two-centre retrospective cohort study. Int J Surg. 2016;30:13–8.
Nagem RG, Lázaro-da-Silva A, de Oliveira RM, et al. Gallstone-related complications after Roux-en-Y gastric bypass: a prospective study. Hepatobiliary Pancreat Dis Int. 2012;11(6):630–5.
Altieri MS, Yang J, Nie L, et al. Incidence of cholecystectomy after bariatric surgery. Surg Obes Relat Dis. 2018;14(7):992–6.
Talha A, Abdelbaki T, Farouk A, et al. Cholelithiasis after bariatric surgery, incidence, and prophylaxis: randomized controlled trial. Surg Endosc. 2020;34(12):5331–7.
O’Brien PE, Dixon JB. A rational approach to cholelithiasis in bariatric surgery. Arch Surg. 2003;138(908):10.1001.
Jonas E, Marsk R, Rasmussen F, et al. Incidence of postoperative gallstone disease after antiobesity surgery: population-based study from Sweden. Surg Obes Relat Dis. 2010;6(1):54–8.
Quesada BM, Kohan G, Roff HE, et al. Management of gallstones and gallbladder disease in patients undergoing gastric bypass. World J Gastroenterol: WJG. 2010;16(17):2075.
Doulamis IP, Michalopoulos G, Boikou V, et al. Concomitant cholecystectomy during bariatric surgery: the jury is still out. Am J Surg. 2019;218(2):401–10.
Guarino MPL, Cocca S, Altomare A, et al. Ursodeoxycholic acid therapy in gallbladder disease, a story not yet completed. World J Gastroenterol: WJG. 2013;19(31):5029.
Van De Heijning BJ, Van De Meeberg PC, Portincasa P, et al. Effects of ursodeoxycholic acid therapy on in vitro gallbladder contractility in patients with cholesterol gallstones. Dig Dis Sci. 1999;44(1):190–6.
Uy MC, Talingdan-Te MC, Espinosa WZ, et al. Ursodeoxycholic acid in the prevention of gallstone formation after bariatric surgery: a meta-analysis. Obes Surg. 2008;18(12):1532–8.
Sharma AHS, Nageswaran H Best L, Patel G A. Role of Ursodeoycholic acid in prevention of gallstones formation in bariatric patients. PROSPERO 2021; https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021276719.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Chinese edition). J Chinese Integr Med. 2009;7(9):889–96.
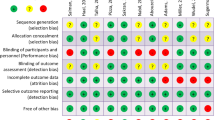
Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Schünemann HJ, Higgins JP, Vist GE, et al. Completing ‘Summary of findings’ tables and grading the certainty of the evidence. Cochrane Handbook for systematic reviews of interventions. 2019:375–402.
Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046–55.
Manager R. In: TC C, editor. 2020.
Higgins JP, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions: Wiley; 2019.
Gurusamy K, Gluud C, Nikolova D, et al. Assessment of risk of bias in randomized clinical trials in surgery. J British Surg. 2009;96(4):342–9.
Sharma A, Rajalingam V, Nageswaran H, et al. A meta-analysis on continuous versus interrupted skin closure following appendicectomy. Br J Surg. 2021;108(8):898–907.
Higgins JP, Li T, Deeks JJ. Choosing effect measures and computing estimates of effect. Cochrane handbook for systematic reviews of interventions. 2019:143–76.
Wallace BC, Dahabreh IJ, Trikalinos TA, et al. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. 2012;49:1–15.
Abouzeid TA, Shoka AA. Should we prescribe ursodeoxycholic acid after laparoscopic sleeve gastrectomy? A two-center prospective randomized controlled trial. Egyptian J Surg. 2018;37(3):349–54.
Adams LB, Chang C, Pope J, et al. Randomized, prospective comparison of ursodeoxycholic acid for the prevention of gallstones after sleeve gastrectomy. Obes Surg. 2016;26(5):990–4.
Haal S, Guman MS, Boerlage TC, et al. Ursodeoxycholic acid for the prevention of symptomatic gallstone disease after bariatric surgery (UPGRADE): a multicentre, double-blind, randomised, placebo-controlled superiority trial. Lancet Gastroenterol Hepatol. 2021;6(12):993–1001.
Hassan MU, Akram MA, Javaid I, et al. Role of ursodeoxycholic acid in prevention of gallstones after sleeve gastrectomy. Pakistan J Med Health Sci. 2021;15(3):666–8.
Miller K, Hell E, Lang B, et al. Gallstone formation prophylaxis after gastric restrictive procedures for weight loss: a randomized double-blind placebo-controlled trial. Ann Surg. 2003;238(5):697.
Nabil TM, Khalil AH, Gamal K. Effect of oral ursodeoxycholic acid on cholelithiasis following laparoscopic sleeve gastrectomy for morbid obesity. Surg Obes Relat Dis. 2019;15(6):827–31.
Pizza F, D’Antonio D, Lucido FS, et al. The role of ursodeoxycholic acid (UDCA) in cholelithiasis management after one anastomosis gastric bypass (OAGB) for morbid obesity: results of a monocentric randomized controlled trial. Obes Surg. 2020;30(11):4315–24.
Sakran N, Dar R, Assalia A, et al. The use of Ursolit for gallstone prophylaxis following bariatric surgery: a randomized-controlled trial. Updat Surg. 2020;72(4):1125–33.
Elshenawy MSI, Ammar MS, Hagag MGE. Effectiveness of using ursodeoxycholic acid in reducing incidence of gallstone formation after sleeve gastrectomy. Int Surg J. 2019;6(2):403–8.
Sugerman HJ, Brewer WH, Shiffman ML, et al. A multicenter, placebo-controlled, randomized, double-blind, prospective trial of prophylactic ursodiol for the prevention of gallstone formation following gastric-bypass-induced rapid weight loss. Am J Surg. 1995;169(1):91–7.
Williams C, Gowan R, Perey BJ. A double-blind placebo-controlled trial of ursodeoxycholic acid in the prevention of gallstones during weight loss after vertical banded gastroplasty. Obes Surg. 1993;3(3):257–9.
Worobetz L, Inglis F, Shaffer E. The effect of ursodeoxycholic acid therapy on gallstone formation in the morbidly obese during rapid weight loss. Am J Gastroenterol. 1993;88(10):1705–1710.
Wudel LJ Jr, Wright JK, Debelak JP, et al. Prevention of gallstone formation in morbidly obese patients undergoing rapid weight loss: results of a randomized controlled pilot study. J Surg Res. 2002;102(1):50–6.
Coupaye M, Castel B, Sami O, et al. Comparison of the incidence of cholelithiasis after sleeve gastrectomy and Roux-en-Y gastric bypass in obese patients: a prospective study. Surg Obes Relat Dis. 2015;11(4):779–84.
Sneineh MA, Harel L, Elnasasra A, et al. Increased incidence of symptomatic cholelithiasis after bariatric Roux-En-Y gastric bypass and previous bariatric surgery: a single center experience. Obes Surg. 2020;30:846–50.
Moon RC, Teixeira AF, DuCoin C, et al. Comparison of cholecystectomy cases after Roux-en-Y gastric bypass, sleeve gastrectomy, and gastric banding. Surg Obes Relat Dis. 2014;10(1):64–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented as an oral abstract at the UGI Congress, Belfast, UK, October 2021
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharma, A., Shanti, H., Nageswaran, H. et al. Role of Ursodeoxycholic Acid in the Prevention of Gallstones Formation in Bariatric Patients—a Systematic Review and Meta-Analysis of Randomised Trials. OBES SURG 33, 4115–4124 (2023). https://doi.org/10.1007/s11695-023-06893-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06893-9