Abstract
Introduction/Purpose
The obesity epidemic is rapidly growing, and visceral adiposity is associated with metabolic consequences secondary to peroxisome proliferator-activated receptor (PPAR)-induced inter-organ signaling pathways. PPARs are ligand-activated transcription factors that modulate vagal pathways which can improve blood pressure, arterial remodeling, cholesterol levels, and insulin sensitivity. However, an obesity-induced inflammatory milieu can interfere with the beneficial effects of PPAR activity, suggesting that a dysregulated PPAR-vagus pathway may play a role in the pathogenesis of obesity-related hypertension. Therefore, we hypothesized that hepatic vagotomy (HV) in patients with obesity would result in a significant reduction in blood pressure and/or the number of hypertension medications compared to control.
Methods
We conducted a retrospective chart review of 160 patients undergoing laparoscopic sleeve gastrectomy. Patients were divided into HV and control groups, and information was collected at each clinic visit.
Results
At six-months post-operation, the HV group was found to have significantly lower total cholesterol (TC)/high-density lipoprotein (HDL) ratios than the control group. The HV group also had a numerically better blood profile for TC, HDL, low-density lipoprotein (LDL), triglycerides, C-reactive protein, and LDL/HDL ratio. Hypertensive patients in the HV group showed numerically lower hypertension medication counts after six weeks when compared to control.
Conclusion
We present the first study to report clinically significant changes related to HV in human subjects. Our results did not support our initial hypothesis but did demonstrate an improvement of the TC/HDL ratio with HV in patients with obesity. Future studies should confirm these findings in a randomized control trial.
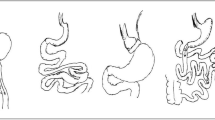
Graphical Abstract

Similar content being viewed by others
References
Uno K, Yamada T, Ishigaki Y, et al. Hepatic peroxisome proliferator-activated receptor-γ-fat-specific protein 27 pathway contributes to obesity-related hypertension via afferent vagal signals. Eur Heart J. 2012;33(10):1279–89. https://doi.org/10.1093/eurheartj/ehr265.
Moreno M, Lombardi A, Silvestri E, et al. PPARs: Nuclear Receptors Controlled by, and Controlling, Nutrient Handling through Nuclear and Cytosolic Signaling. PPAR Res. 2010;2010:435689. https://doi.org/10.1155/2010/435689
Wilson JL, Duan R, El-Marakby A, et al. Peroxisome Proliferator Activated Receptor-α Agonist Slows the Progression of Hypertension, Attenuates Plasma Interleukin-6 Levels and Renal Inflammatory Markers in Angiotensin II Infused Mice. PPAR Res. 2012;2012:645969. https://doi.org/10.1155/2012/645969.
Zarzuelo MJ, Jiménez R, Galindo P, et al. Antihypertensive effects of peroxisome proliferator-activated receptor-β activation in spontaneously hypertensive rats. Hypertension. 2011;58(4):733–43. https://doi.org/10.1161/HYPERTENSIONAHA.111.174490.
Botta M, Audano M, Sahebkar A, et al. PPAR Agonists and Metabolic Syndrome: An Established Role? Int J Mol Sci. 2018;19(4):1197. https://doi.org/10.3390/ijms19041197.
Usuda D, Kanda T. Peroxisome proliferator-activated receptors for hypertension. World J Cardiol. 2014;6(8):744–54. https://doi.org/10.4330/wjc.v6.i8.744.
Westerbacka J, Kolak M, Kiviluoto T, et al. Genes involved in fatty acid partitioning and binding, lipolysis, monocyte/macrophage recruitment, and inflammation are overexpressed in the human fatty liver of insulin-resistant subjects. Diabetes. 2007;56(11):2759–65. https://doi.org/10.2337/db07-0156.
Bernal-Mizrachi C, Xiaozhong L, Yin L, et al. An afferent vagal nerve pathway links hepatic PPARalpha activation to glucocorticoid-induced insulin resistance and hypertension. Cell Metab. 2007;5(2):91–102. https://doi.org/10.1016/j.cmet.2006.12.010.
Pham GS, Shimoura CG, Chaudhari S, et al. Chronic unilateral cervical vagotomy reduces renal inflammation, blood pressure, and renal injury in a mouse model of lupus. Am J Physiol Renal Physiol. 2020;319(2):F155-F161. https://doi.org/10.1152/ajprenal.00201.2020.
Lubaczeuski C, Balbo SL, Ribeiro RA, et al. Vagotomy ameliorates islet morphofunction and body metabolic homeostasis in MSG-obese rats. Braz J Med Biol Res. 2015;48(5):447–57. https://doi.org/10.1590/1414-431X20144340.
Souza-Mello V. Peroxisome proliferator-activated receptors as targets to treat non-alcoholic fatty liver disease. World J Hepatol. 2015;7(8):1012–9. https://doi.org/10.4254/wjh.v7.i8.1012.
Purdy M, Nykopp TK, Kainulainen S, et al. Division of the hepatic branch of the anterior vagus nerve in fundoplication: effects on gallbladder function. Surg Endosc. 2009;23(9):2143–6. https://doi.org/10.1007/s00464-008-0242-0.
Woodward ER. The history of vagotomy. Am J Surg. 1987;153(1):9–17. https://doi.org/10.1016/0002-9610(87)90195-4.
Rabben HL, Zhao CM, Hayakawa Y, et al. Vagotomy and Gastric Tumorigenesis. Curr Neuropharmacol. 2016;14(8):967–72. https://doi.org/10.2174/1570159x14666160121114854.
Seeras K, Qasawa RN, Prakash S. Truncal Vagotomy. Tampa, FL: StatPearls; 2021.
Centers for Disease Control and Prevention. 2021 Sept 30. Adult Obesity Facts. Retrieved October 11, 2021 from https://www.cdc.gov/obesity/data/adult.html.
Bocher V, Pineda-Torra I, Fruchart JC, et al. PPARs: transcription factors controlling lipid and lipoprotein metabolism. Ann N Y Acad Sci. 2002;967:7–18. https://doi.org/10.1111/j.1749-6632.2002.tb04258.x.
Chao L, Marcus-Samuels B, Mason MM, et al. Adipose tissue is required for the antidiabetic, but not for the hypolipidemic, effect of thiazolidinediones. J Clin Invest. 2000;106(10):1221–8. https://doi.org/10.1172/JCI11245.
Rahimian R, Masih-Khan E, Lo M, et al. Hepatic over-expression of peroxisome proliferator activated receptor gamma2 in the ob/ob mouse model of non-insulin dependent diabetes mellitus. Mol Cell Biochem. 2001;224(1–2):29–37. https://doi.org/10.1023/a:1011927113563.
Uno K, Katagiri H, Yamada T, et al. Neuronal pathway from the liver modulates energy expenditure and systemic insulin sensitivity. Science. 2006;312(5780):1656–9. https://doi.org/10.1126/science.1126010.
Ferrer-Márquez M, Belda-Lozano R, Ferrer-Ayza M. Technical Controversies in Laparoscopic Sleeve Gastrectomy. OBES SURG. 2012;22:182–7. https://doi.org/10.1007/s11695-011-0492-0.
Picone DS, Schultz MG, Otahal P, et al. Accuracy of Cuff-Measured Blood Pressure: Systematic Reviews and Meta-Analyses. J Am Coll Cardiol. 2017;70(5):572–86. https://doi.org/10.1016/j.jacc.2017.05.064.
Schiavon CA, Bersch-Ferreira AC, Santucci EV, et al. Effects of Bariatric Surgery in Obese Patients With Hypertension: The GATEWAY Randomized Trial (Gastric Bypass to Treat Obese Patients With Steady Hypertension). Circulation. 2018;137(11):1132–1142. https://doi.org/10.1161/CIRCULATIONAHA.117.032130. Erratum in: Circulation. 2019 Oct;140(14):e718.
Wen J, Huang Y, Lu Y, et al. Associations of non-high-density lipoprotein cholesterol, triglycerides and the total cholesterol/HDL-c ratio with arterial stiffness independent of low-density lipoprotein cholesterol in a Chinese population. Hypertens Res. 2019;42(8):1223–1230. https://doi.org/10.1038/s41440-019-0251-5.
Ingelsson E, Schaefer EJ, Contois JH, et al. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA. 2007;298(7):776–85. https://doi.org/10.1001/jama.298.7.776.
Acknowledgements
We thank Dr. Frank Greenway at Pennington Biomedical Research Center (Baton Rouge, LA) for assisting us with the study design.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. Hepatic vagotomy results in lower total cholesterol/high-density lipoprotein ratios.
2. Hepatic vagotomy may reverse obesity related dysregulation of hepatic PPAR activity.
3. Hepatic vagotomy enhances bariatric surgery's positive impact on CRP & TC/HDL.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Catinis, A.M., Hinojosa, A.J., Leonardi, C. et al. Hepatic Vagotomy in Patients With Obesity Leads to Improvement of the Cholesterol to High-Density Lipoprotein Ratio. OBES SURG 33, 3740–3745 (2023). https://doi.org/10.1007/s11695-023-06800-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06800-2