Abstract
Purpose
One-anastomosis gastric bypass (OAGB) is a relatively simple surgical procedure for those afflicted with severe obesity. Studies reported symptomatic biliary reflux gastritis and esophagitis as predominant complications. Hepatobiliary scintigraphy (HIDA) is the least invasive test for the diagnosis of bile reflux, with good sensitivity, patient tolerability, and reproducibility. The aim of this study was to define an optimized HIDA scintigraphy protocol for demonstrating bile reflux in post-OAGB patients.
Material and Methods
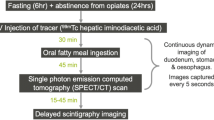
We conducted a prospective multicenter study. Patients after OAGB with dyspeptic complaints were included. All patients underwent HIDA scan with a dedicated protocol for demonstrating bile reflux; prevalence and severity were reported.
Results
Nineteen patients were included, 18 females and one male, with mean age of 41.8 years and mean time of 22.4 months from operation to the scan. Bile reflux into the gastric pouch was documented in 11 patients (53%). Reflux to the stomach pouch was severe in three patients (27%), moderate in two patients (18%), and mild in six patients (55%). Bile reflux into the esophagus was documented in four patients (21%), severe reflux in one patient (25%), and mild in the other three (75%). A correlation was found between complaints of vomiting, heartburn and regurgitation, and findings of esophagitis on gastroscopy in patients with vs. without reflux.
Conclusions
The tailored HIDA scan protocol detected bile reflux in more than half of the post-OAGB patients included in the study, with a high diagnostic sensitivity.
Graphical Abstract





Similar content being viewed by others
Abbreviations
- OAGB:
-
One-anastomosis gastric bypass
- HIDA:
-
Hepatobiliary scintigraphy
- BMI:
-
Body mass index
- RYGB:
-
Roux-En-Y gastric bypass
- DGER:
-
Duodenogastroesophageal reflux
- SPECT:
-
Single-photon emission computerized tomography
- CT:
-
Computed tomography
- SD:
-
Standard deviation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- PPI:
-
Proton pump inhibitors
References
Rutledge R, Kular K, Manchanda N. The mini-gastric bypass original technique. Int J Surg. 2019;61:38–41.
Rutledge R. Hospitalization before and after mini-gastric bypass surgery. Int J Surg. 2007;5:35–40.
Wang W, Wei PL, Lee YC, et al. Short-term results of laparoscopic mini-gastric bypass. Obes Surg. 2005;15:648–54.
Jung JJ, Park AK, Hutter MM. The United States experience with one anastomosis gastric bypass at MBSAQIP-accredited centers. Obes Surg. 2022;32:3239–47.
Johnson WH, Fernanadez AZ, Farrell TM, et al. Surgical revision of loop ("mini") gastric bypass procedure: multicenter review of complications and conversions to Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2007;3:37–41.
Chen X, Oshima T, Tomita T, et al. Acidic bile salts modulate the squamous epithelial barrier function by modulating tight junction proteins. Am J Physiol Gastrointest Liver Physiol. 2011;301:G203–9.
Gillen P, Keeling P, Byrne PJ, et al. Implication of duodenogastric reflux in the pathogenesis of Barrett's oesophagus. Br J Surg. 1988;75:540–3.
Eldredge TA, Myers JC, Kiroff GK, et al. Detecting bile reflux-the enigma of bariatric surgery. Obes Surg. 2018;28:559–66.
Mittal BR, Ibrarullah M, Agarwal DK, et al. Comparative evaluation of scintigraphy and upper gastrointestinal tract endoscopy for detection of duodenogastric reflux. Ann Nucl Med. 1994;8:183–6.
Chen TF, Yadav PK, Wu RJ, et al. Comparative evaluation of intragastric bile acids and hepatobiliary scintigraphy in the diagnosis of duodenogastric reflux. World J Gastroenterol. 2013;19:2187–96.
Tulchinsky M, Ciak BW, Delbeke D, et al. SNM practice guideline for hepatobiliary scintigraphy 4.0. J Nucl Med Technol. 2010;38:210–8.
Shaffer EA, McOrmond P, Duggan H. Quantitative cholescintigraphy: assessment of gallbladder filling and emptying and duodenogastric reflux. Gastroenterology. 1980;79:899–906.
Mahawar KK, Kumar P, Carr WR, et al. Current status of mini-gastric bypass. J Minim Access Surg. 2016;12:305–10.
Deitel M, Rutledge R. Mini-gastric bypass: prevention and management of complications in performance and follow-up. Int J Surg. 2019;71:119–23.
Barrett MW, Myers JC, Watson DI, et al. Detection of bile reflux: in vivo validation of the Bilitec fibreoptic system. Dis Esophagus. 2000;13:44–50.
Just RJ, Leite LP, Castell DO. Changes in overnight fasting intragastric pH show poor correlation with duodenogastric bile reflux in normal subjects. Am J Gastroenterol. 1996;91:1567–70.
Stein HJ, Smyrk TC, DeMeester TR, et al. Clinical value of endoscopy and histology in the diagnosis of duodenogastric reflux disease. Surgery. 1992;112:796–803. discussion 803-4
Muhammed I, McLoughlin GP, Holt S, et al. Non-invasive estimation of duodenogastric reflux using technetium-99m p-butyl-iminodiacetic acid. Lancet. 1980;2:1162–5.
Mackie CR, Wisbey ML, Cuschieri A. Milk 99Tcm-EHIDA test for enterogastric bile reflux. Br J Surg. 1982;69:101–4.
Sorgi M, Wolverson RL, Mosimann F, et al. Sensitivity and reproducibility of a bile reflux test using 99mTc HIDA. Scand J Gastroenterol Suppl. 1984;92:30–2.
Padhy AK, Losu V, Shukla NK, et al. Thoracic stomach: comparative evaluation of endoscopy, gastric aspirate analysis and hepatobiliary scintigraphy in the diagnosis of duodeno-gastric reflux. Indian J Gastroenterol. 1990;9:277–9.
Keleidari B, Mahmoudieh M, Davarpanah Jazi AH, et al. Comparison of the bile reflux frequency in one anastomosis gastric bypass and Roux-en-Y gastric bypass: a cohort study. Obes Surg. 2019;29:1721–5.
Shenouda MM, Harb SE, Mikhail SAA, et al. Bile gastritis following laparoscopic single anastomosis gastric bypass: pilot study to assess significance of bilirubin level in gastric aspirate. Obes Surg. 2018;28:389–95.
Saarinen T, Rasanen J, Salo J, et al. Bile reflux scintigraphy after mini-gastric bypass. Obes Surg. 2017;27:2083–9.
Saarinen T, Pietilainen KH, Loimaala A, et al. Bile reflux is a common finding in the gastric pouch after one anastomosis gastric bypass. Obes Surg. 2020;30:875–81.
Eldredge TA, Bills M, Myers JC, et al. HIDA and seek: challenges of scintigraphy to diagnose bile reflux post-bariatric surgery. Obes Surg. 2020;30:2038–45.
Eldredge TA, Bills M, Ting YY, et al. Once in a bile - the incidence of bile reflux post-bariatric surgery. Obes Surg. 2022;32:1428–38.
Sifrim D, Castell D, Dent J, et al. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024–31.
Acknowledgements
We would like to thank Mr. Akram Akawi, the head technologist in the Nuclear Medicine Department, for his contribution in the development of the scan protocol and his dedicated work in performing the scans.
Author information
Authors and Affiliations
Contributions
Elite Arnon-Sheleg, Tawfik Khoury, and Wisam Sbeit contributed to the study concept and design. Wisam Sbeit, Moaad Faraj, and Amir Mari contributed to patients’ recruitment. Tawfik Khoury and Samar Michael analyzed the data and wrote the first version of the manuscript. Elite Arnon-Sheleg, Tawfik Khoury, and Wisam Sbeit critically reviewed the manuscript for publication readiness. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Ethical Approval and Consent to Participate
The trial was reviewed by the operative ethics committee and approved by the scientific board of our institutions. The study was carried out according to the Helsinki Declaration and informed consent was obtained from all patients.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
-One-anastomosis gastric bypass (OAGB) surgery is increasingly used for bariatric surgery.
-Few studies suggest its association with bile reflux; to date, there is no standard, well-tolerated study used to diagnose bile reflux.
-Our novel HIDA protocol identified bile reflux in more than half of the patients.
-Bile reflux mostly correlated with vomiting, heartburn, and regurgitation.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arnon-Sheleg, E., Farraj, M., Michael, S. et al. Modified Hepatobiliary Scintigraphy for the Diagnosis of Bile Reflux in One-Anastomosis Gastric Bypass Surgery: a Prospective Multicenter Study. OBES SURG 33, 1997–2004 (2023). https://doi.org/10.1007/s11695-023-06632-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06632-0