Abstract
Purpose
Resectional Roux-en-Y gastric bypass (RRYGB) is considered an alternative bariatric surgery in countries with a high incidence of stomach cancer because there is no excluded stomach after RRYGB. This study aimed to evaluate the efficacy and safety of RRYGB.
Materials and Methods
This study included patients who underwent RRYGB and sleeve gastrectomy (SG) between 2011 and 2021. Surgical complications and metabolic and nutritional profiles were compared between the patients preoperatively and at 1, 6, and 12 months after surgery.
Results
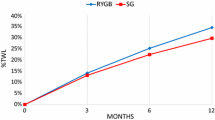
Twenty and seventy-six patients underwent RRYGB and SG, respectively; 7 in the SG group were lost to follow-up within 1 year. Surgical complications and baseline characteristics were comparable between two groups, except for diabetes (90.0% vs. 44.7%, p < 0.001). The decrease of HbA1c levels and incidence of reflux esophagitis were lower in the RRYGB group compared to that of SG at 1-year postoperative (-3.0% vs. -1.8%, p = 0.014; 0% vs. 26.7%, p = 0.027). The percentage of total weight loss at 1- year postoperative and incidence of dumping syndrome were comparable between the two groups. The RRYGB group had significantly lower total cholesterol level (161.9 mg/dl vs. 196.4 mg/dl, p < 0.001), but higher incidence of vitamin B12 deficiency (30.0% vs. 3.6%, p = 0.003) at 1 year postoperative compared to those of the SG group.
Conclusions
The RRYGB group had better postoperative outcomes for diabetes and dyslipidemia without increasing surgical complications compared to that of the SG group. Thus, RRYGB can be considered a safe and effective alternative in areas where gastric cancer is prevalent.
Graphical Abstract




Similar content being viewed by others
Data Availability
The data that support the findings of this study are available on request from the corresponding author.
References
Park DJ, An S, Park YS, et al. Bariatric surgery versus medical therapy in Korean obese patients: prospective multicenter nonrandomized controlled trial (KOBESS trial). Ann Surg Treat Res. 2021;101(4):197–205.
Oh TJ, Lee HJ, Cho YM. East Asian perspectives in metabolic and bariatric surgery. J Diabetes Investig. 2022;13(5):756–61.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Park SH, Kang MJ, Yun EH, et al. Epidemiology of gastric cancer in Korea: trends in incidence and survival based on korea central cancer registry data (1999–2019). J Gastric Cancer. 2022;22(3):160–8.
Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–75.
Elton E, Hanson BL, Qaseem T, et al. Diagnostic and therapeutic ERCP using an enteroscope and a pediatric colonoscope in long-limb surgical bypass patients. Gastrointest Endosc. 1998;47(1):62–7.
Silecchia G, Catalano C, Gentileschi P, et al. Virtual gastroduodenoscopy: a new look at the bypassed stomach and duodenum after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2002;12(1):39–48.
Curry TK, Carter PL, Porter CA, et al. Resectional gastric bypass is a new alternative in morbid obesity. Am J Surg. 1998;175(5):367–70.
Park JY, Kim YJ. Laparoscopic resectional gastric bypass: initial experience in morbidly obese Korean patients. Surg Today. 2015;45(8):1032–9.
Parrott J, Frank L, Rabena R, et al. American society for metabolic and bariatric surgery integrated health nutritional guidelines for the surgical weight loss patient 2016 update: micronutrients. Surg Obes Relat Dis. 2017;13(5):727–41.
Leahy CR, Luning A. Review of nutritional guidelines for patients undergoing bariatric surgery. AORN J. 2015;102(2):153–60.
Grong E, Arbo IB, Thu OK, et al. The effect of duodenojejunostomy and sleeve gastrectomy on type 2 diabetes mellitus and gastrin secretion in Goto-Kakizaki rats. Surg Endosc. 2015;29(3):723–33.
Sillakivi T, Suumann J, Kirsimagi U, et al. Plasma levels of gastric biomarkers in patients after bariatric surgery: biomarkers after bariatric surgery. Hepatogastroenterology. 2013;60(128):2129–32.
Lee KG, Lee HJ, Yang JY, et al. Risk factors associated with complication following gastrectomy for gastric cancer: retrospective analysis of prospectively collected data based on the Clavien-Dindo system. J Gastrointest Surg. 2014;18(7):1269–77.
Lee WJ, Hur KY, Lakadawala M, et al. Predicting success of metabolic surgery: age, body mass index, C-peptide, and duration score. Surg Obes Relat Dis. 2013;9(3):379–84.
Aminian A, Brethauer SA, Andalib A, et al. Individualized metabolic surgery score: procedure selection based on diabetes severity. Ann Surg. 2017;266(4):650–7.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5.
Hong S, Won YJ, Lee JJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2018. Cancer Res Treat. 2021;53(2):301–15.
Kang SH, Lee Y, Park YS, et al. Solo single-incision laparoscopic resectional Roux-en-Y gastric bypass for morbid obesity with metabolic syndrome. Obes Surg. 2017;27(12):3314–9.
Kumar SB, Hamilton BC, Wood SG, et al. Is laparoscopic sleeve gastrectomy safer than laparoscopic gastric bypass? A comparison of 30-day complications using the MBSAQIP data registry. Surg Obes Relat Dis. 2018;14(3):264–9.
Surve A, Cottam D, Richards C, et al. A matched cohort comparison of long-term outcomes of Roux-en-Y gastric bypass (RYGB) versus Single-anastomosis duodeno-ileostomy with sleeve gastrectomy (SADI-S). Obes Surg. 2021;31(4):1438–48.
Wiggins T, Pournaras DJ, Priestman E, et al. Effect of preoperative weight loss and baseline comorbidity on short-term complications and reoperations after laparoscopic Roux-en-Y gastric bypass in 2,067 patients. Obes Surg. 2021;31(6):2444–52.
Nguyen NT, Varela E, Sabio A, et al. Resolution of hyperlipidemia after laparoscopic Roux-en-Y gastric bypass. J Am Coll Surg. 2006;203(1):24–9.
Cowan GS Jr, Buffington CK. Significant changes in blood pressure, glucose, and lipids with gastric bypass surgery. World J Surg. 1998;22(9):987–92.
Brolin RE, Bradley LJ, Wilson AC, et al. Lipid risk profile and weight stability after gastric restrictive operations for morbid obesity. J Gastrointest Surg. 2000;4(5):464–9.
Lewis CA, de Jersey S, Seymour M, et al. Iron, vitamin B12, folate and copper deficiency after bariatric surgery and the impact on anaemia: a systematic review. Obes Surg. 2020;30(11):4542–91.
Yale CE, Gohdes PN, Schilling RF. Cobalamin absorption and hematologic status after two types of gastric surgery for obesity. Am J Hematol. 1993;42(1):63–6.
Ahmad A, Kornrich DB, Krasner H, et al. Prevalence of dumping syndrome after laparoscopic sleeve gastrectomy and comparison with laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2019;29(5):1506–13.
Lewis KH, Arterburn DE, Zhang F, et al. Comparative effectiveness of vertical sleeve gastrectomy versus Roux-en-Y gastric bypass for diabetes treatment: a claims-based cohort study. Ann Surg. 2021;273(5):940–8.
Huh YJ, Son YG, Kim TH, et al. Effect and mechanisms of diabetes resolution according to the range of gastric resection and the length of anastomosis in animal models: implication for gastric cancer surgery in patients with diabetes mellitus. World J Surg. 2018;42(4):1056–64.
Hofso D, Fatima F, Borgeraas H, et al. Gastric bypass versus sleeve gastrectomy in patients with type 2 diabetes (Oseberg): a single-centre, triple-blind, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7(12):912–24.
Ha J, Jang M, Kwon Y, et al. Metabolomic Profiles Predict Diabetes Remission after Bariatric Surgery. J Clin Med. 2020;9(12):3897
Jun JK, Choi KS, Lee HY, et al. Effectiveness of the Korean national cancer screening program in reducing gastric cancer mortality. Gastroenterology. 2017;152(6):1319-28 e7.
Funding
This study was supported by grants from National Evidence-based Healthcare Collaborating Agency (grant number: HC21C0099) funded by the Ministry of Health & Welfare, Republic of Korea. The funder had no role in study design, data collection, analysis and interpretation or manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cho, YS., Park, JH., Kim, J. et al. Clinical Outcomes of Resectional Roux-en-Y Gastric Bypass, Compared to Sleeve Gastrectomy for Severe Obesity. OBES SURG 33, 1338–1346 (2023). https://doi.org/10.1007/s11695-023-06544-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06544-z



