Abstract
Background
Obesity is a widely prevalent medical and socioeconomic problem. Bariatric surgery is indicated for patients with clinically severe obesity. Reduction of gastric volume is an important factor that contributes to weight loss after laparscopic sleeve gastrectomy (LSG). The impact of the gastric volume on weight after LSG has been studied.
Aim of the Study
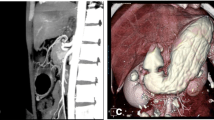
This study was designed to assess the gastric volume in patients with obesity prior to LSG and in the normal-weight patients, using three-dimensional multi-detector computer tomography (3D-MDCT), and to evaluate the potential correlation of the gastric volume with body mass index (BMI).
Patients and Methods
A total of 100 patients were equally enrolled in two groups: one group for patients with obesity scheduled for LSG and another one for normal-weight patients scheduled for non-bariatric surgery. The study patients underwent 3D-MDCT gastric volumetry.
Results
The gastric volume ranged from 525 to 1170 mL in patients with obesity and from 312 to 676 mL in the normal-weight group. Statistically significant difference was found between the two groups. Age, weight, and BMI were found to be predictors for the gastric volume in normal-weight patients only.
Conclusion
MDCT gastric volumetry is a feasible method to assess the stomach volume. Higher volumes were evident in patients with obesity. Age, weight, and BMI are predictors for the gastric volume in normal-weight patients with linear regression equations that could help during the preoperative planning of bariatric surgeries.
Graphical Abstract




Similar content being viewed by others
References
Pantalone KM, Hobbs TM, Chagin KM, et al. Prevalence and recognition of obesity and its associated comorbidities: cross-sectional analysis of electronic health record data from a large US integrated health system. BMJ Open. 2017;7: e017583.
Soong T-C, Lee M-H, Lee W-J, et al. Long-term efficacy of bariatric surgery for the treatment of super-obesity: comparison of SG, RYGB, and OAGB. Obes Surg. 2021;31:3391–9.
Lee M-H, Almalki OM, Lee W-J, et al. Laparoscopic sleeve gastrectomy for type 2 diabetes mellitus: long-term result and recurrence of diabetes. Obes Surg. 2020;30:3669–74.
Paluszkiewicz R, Kalinowski P, Wróblewski T, et al. Prospective randomized clinical trial of laparoscopic sleeve gastrectomy versus open Roux-en-Y gastric bypass for the management of patients with morbid obesity. Wideochir Inne Tech Maloinwazyjne. 2012;7(4):225–32.
Benaiges D, Más-Lorenzo A, Goday A, et al. Laparoscopic sleeve gastrectomy: more than a restrictive bariatric surgery procedure? World J Gastroenterol. 2015;21(41):11804–14.
Elbanna H, Emile S, El-Hawary GE-S, et al. Assessment of the correlation between preoperative and immediate postoperative gastric volume and weight loss after sleeve gastrectomy using computed tomography volumetry. World J Surg. 2019;43:199–206.
Salman MA, Elshazli M, Shaaban M, et al. Correlation between preoperative gastric volume and weight loss after laparoscopic sleeve gastrectomy. IJGM Dove Press. 2021;14:8135–40.
El Ansari W, Elhag W. Weight regain and insufficient weight loss after bariatric surgery: definitions, prevalence, mechanisms, predictors, prevention and management strategies, and knowledge gaps—a scoping review. Obes Surg. 2021;31:1755–66.
Horton KM, Fishman EK. Current role of CT in imaging of the stomach. RadioGraphics Radiol Soc N Am. 2003;23:75–87.
Huh J, Lee I-S, Kim KW, et al. CT gastrography for volumetric measurement of remnant stomach after distal gastrectomy: a feasibility study. Abdom Radiol. 2016;41:1899–905.
Ahmed OE, Refaat M, Shalaan A. The role of 3D-MSCT gastric pouch volumetric study in sleeve gastrectomy. Benha Med J. 2020;36:107–15 (Benha University, Faculty of Medicine).
Kim SH, Keum B, Choi HS, et al. Stomach volume assessment using three-dimensional computed tomography gastrography for bariatric treatment. Obes Surg. 2020;30:401–6.
Hoad CL, Parker H, Hudders N, et al. Measurement of gastric meal and secretion volumes using magnetic resonance imaging. Phys Med Biol. 2015;60(3):1367–83.
Deslandes A. Sonographic demonstration of stomach pathology: reviewing the cases. Australas J Ultrasound Med. 2013;16(4):202–9.
Blanchet MC, Mesmann C, Yanes M, et al. 3D gastric computed tomography as a new imaging in patients with failure or complication after bariatric surgery. Obes Surg. 2010;20(12):1727–33.
Alva S, Eisenberg D, Duffy A, et al. Virtual three-dimensional computed tomography assessment of the gastric pouch following laparoscopic Roux-Y gastric bypass. Obes Surg. 2008;18(4):364–6.
Deloose E, Janssen P, Depoortere I, et al. The migrating motor complex: control mechanisms and its role in health and disease. Nat Rev Gastroenterol Hepatol. 2012;9(5):271–85.
Geliebter A. Stomach capacity in obese individuals. Obes Res. 2001;9:727–8.
Mohammad Khalil A, GaberRagab S, MakramBotros J, et al. Gastric residual volume assessment by gastric ultrasound in fasting obese patients: a comparative study. Anesth Pain Med. 2021;11: e109732.
Izquierdo AG, Crujeiras AB, Casanueva FF, et al. Leptin, obesity, and leptin resistance: where are we 25 years later? Nutrients. 2019;11(11):2704.
Tsani A, Widowati A, Dieny F, et al. Satiety profiles in obese and normal adults after high-carbohydrate diet ingestion. Pak J Med Health Sci. 2021;15:2051–5.
Pegington M, French DP, Harvie MN. Why young women gain weight: a narrative review of influencing factors and possible solutions. Obes Rev. 2020;21: e13002.
Xiao X, Wang W, Sa R, et al. The investigation of sex differences in the effect of body mass index. Int J Hypertens. 2019;2019:e1360328 (Hindawi).
Álvarez-Castro P, Pena L, Cordido F. Ghrelin in obesity, physiological and pharmacological considerations. Mini Rev Med Chem. 2013;13:541–52.
Anderson B, Switzer NJ, Almamar A, et al. The impact of laparoscopic sleeve gastrectomy on plasma ghrelin levels: a systematic review. Obes Surg. 2013;23:1476–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed were in accordance with the ethical standards of the institutional research committee and with the Helsinki declaration.
Conflict of Interest
The authors declare no competing interests.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
(1) Obesity is a widely prevalent medical and socioeconomic problem.
(2) Laparoscopic sleeve gastrectomy (LSG) is presently one of the most popular bariatric techniques thanks to several reports on its promising outcomes.
(3) Three dimensional multi-detector computed tomography (3D-MDCT) gastric volumetry has been adopted as the most accurate method for assessment of the stomach volume after surgery.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salman, M.A., Othman, B., Elshehry, A. et al. Three-Dimensional Multi-detector Computed Tomography (3D-MDCT) Gastric Volumetry in Patients with obesity and Normal-Weight Individuals. OBES SURG 33, 418–425 (2023). https://doi.org/10.1007/s11695-022-06402-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06402-4