Abstract
Purpose
This study aimed to compare self-management after bariatric surgery between support group participants (the study group) and patients receiving only individual follow-up by a dietitian (the comparison group), and to examine the differences between the two groups regarding the associations of cognitive and emotional factors with self-management.
Materials and Methods
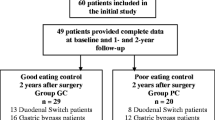
This cross-sectional comparative study was conducted among bariatric patients who either participated in bariatric support groups during the years 2018–2020 or received only individual follow-up with a dietitian since their surgery. The structured questionnaire included a self-management questionnaire, cognitive variables (eating self-efficacy, eating awareness as independent variables, weight control motivation) and emotional variables (positive and negative affect, emotional eating), and background control variables.
Results
The level of self-management was better in the study group than in the comparison group. The hierarchical regression model showed that in the study group, the control variables contributed negligibly to self-management (step 1), while all independent variables contributed the most (27%) to the explained variance (31%) in self-management (step 2). In the comparison group, the contribution of the control variables was 11.5% of the explained variance, with only lower duration of time since surgery being related to higher self-management (step 1). The independent variables contributed significantly — an additional 14.5% to the explained variance (step 2). Emotional eating was the sole variable related to self-management.
Conclusion
The findings emphasize the importance of encouraging patients after bariatric surgery to participate in support groups, as the skills acquired in these groups strengthen the capacity to manage self-care.
Graphical abstract

Similar content being viewed by others
References
Weir CB, Jan A. BMI classification percentile and cut off points. In: StatPearls. Treasure Island (FL): StatPearls Publishing. 2021.
World Health Organization. Obesity and overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 1/4/2022.
Yeo D, Yeo C, Low TY, et al. Outcomes after metabolic surgery in Asians—a meta-analysis. Obes Surg. 2019;29(1):114–26. https://doi.org/10.1007/s11695-018-3484-5.
Arterburn DE, Telem DA, Kushner RF, et al. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324(9):879–887.
Hood MM, Corsica J, Bradley L, et al. Managing severe obesity: understanding and improving treatment adherence in bariatric surgery. J Behav Med. 2016;39(6):1092–103. https://doi.org/10.1007/s10865-016-9772-4.
Sobhani Z, Amini M, Zarnaghash M, et al. Self-management behaviors in obese patients undergoing surgery based on general and specific adherence scales. World J Plast Surg. 2019;8(1):85–92. https://doi.org/10.29252/wjps.8.1.85.
Jones L, Cleator J, Yorke J. Maintaining weight loss after bariatric surgery: when the spectator role is no longer enough. Clin Obes. 2016;6(4):249–58. https://doi.org/10.1111/cob.12152.
Keren D, Matter I, Rainis T. Sleeve gastrectomy in different age groups: a comparative study of 5-year outcomes. Obes Surg. 2016;26(2):289–95. https://doi.org/10.1007/s11695-015-1735-2.
Khorgami Z, Zhang C, Messiah SE, et al. Predictors of postoperative aftercare attrition among gastric bypass patients. Bariatr Surg Pract Patient Care. 2015;10(2):79–83. https://doi.org/10.1089/bari.2014.0053.
Hasan B, Nayfeh T, Alzuabi M, et al. Weight loss and serum lipids in overweight and obese adults: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2020;105(12):dgaa673. https://doi.org/10.1210/clinem/dgaa673.
Pyykkö JE, Aydin Ö, Gerdes VEA, et al. Psychological functioning and well-being before and after bariatric surgery; what is the benefit of being self-compassionate? Br J Health Psychol. 2022;27(1):96–115. https://doi.org/10.1111/bjhp.
Gallé F, Marte G, Cirella A, et al. An exercise-based educational and motivational intervention after surgery can improve behaviors, physical fitness and quality of life in bariatric patients. PLoS One. 2020;15(10):e0241336. https://doi.org/10.1371/journal.pone.0241336.
Bradley LE, Forman EM, Kerrigan SG, et al. A pilot study of an acceptance-based behavioral intervention for weight regain after bariatric surgery. Obes Surg. 2016;26(10):2433–41. https://doi.org/10.1007/s11695-016-2125-0.
Kalarchian MA, Marcus MD. Psychosocial concerns following bariatric surgery: current status. Curr Obes Rep. 2019;8(1):1–9. https://doi.org/10.1007/s13679-019-0325-3.
Livhits M, Mercado C, Yermilov I, et al. Is social support associated with greater weight loss after bariatric surgery?: a systematic review. Obes Rev. 2011;12(2):142–8. https://doi.org/10.1111/j.1467-789X.2010.00720.x.
Andreu A, Jimenez A, Vidal J, et al. Bariatric support groups predicts long-term weight loss. Obes Surg. 2020;30(6):2118–23. https://doi.org/10.1007/s11695-020-04434-2.
Opolski M, Winefield H, Howell C, et al. Banding together: an investigation of post-surgery support groups for laparoscopic adjustable gastric banding patients. Health Psychol Res. 2014;2(2):1464. https://doi.org/10.4081/hpr.2014.1464.
Hameed S, Salem V, Tan TM, et al. Beyond weight loss: establishing a post-bariatric surgery patient support group—what do patients want? J Obes. 2018. https://doi.org/10.1155/2018/8419120.
Chernichovsky D. The Israeli healthcare system: an overview. A chapter from the state of the nation report, 2018. Available online: https://www.taubcenter.org.il/wp-content/uploads/2020/12/healthcareoverview2018en.pdf. Accessed 15 Apr 2022.
Israeli Ministry of Health. National registrar of bariatric surgery. 2019. Retrieved from: https://www.health.gov.il/PublicationsFiles/Bariatric_2018.pdf. Accessed 29 Apr 2022.
Ben-Porat T, Mashin L, Kaluti D, et al. Weight loss outcomes and lifestyle patterns following sleeve gastrectomy: an 8-year retrospective study of 212 patients. Obes Surg. 2021;31(11):4836–45. https://doi.org/10.1007/s11695-021-05650-0.
Endevelt R, Ben-Assuli O, Klain E, et al. The role of dietitian follow-up in the success of bariatric surgery. Surg Obes Relat Dis. 2013;9(6):963–8. https://doi.org/10.1016/j.soard.2013.01.006.
Sherf Dagan S, Keidar A, Raziel A, et al. Do bariatric patients follow dietary and lifestyle recommendations during the first postoperative year? Obes Surg. 2017;27(9):2258–71. https://doi.org/10.1007/s11695-017-2633-6.
Shinan-Altman S, Sandbank GK, Katzav HN, Soskolne V. Participating in bariatric support groups: the effects on self-management changes. Int J Behav Med. 2022. https://doi.org/10.1007/s12529-022-10066-w.
Sherf Dagan S, Goldenshluger A, Globus I, Schweiger C, Kessler Y, Kowen Sandbank G, Ben-Porat T, Sinai T. Nutritional recommendations for adult bariatric surgery patients: clinical practice. Adv Nutr. 2017;8(2):382–94. https://doi.org/10.3945/an.116.014258.
Welch G, Wesolowski C, Piepul B, Kuhn J, Romanelli J, Garb J. Physical activity predicts weight loss following gastric bypass surgery: findings from a support group survey. Obes Surg. 2008;18(5):517–24. https://doi.org/10.1007/s11695-007-9269-x.
Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59(5):739–44. https://doi.org/10.1037//0022-006x.59.5.739.
Stotland S, Larocque M, Sadikaj G. Positive and negative dimensions of weight control motivation. Eat Behav. 2012;13(1):20–6. https://doi.org/10.1016/j.eatbeh.2011.10.003.
Bradburn MM. The structure of psychological well-being. Chicago: Aldine; 1969.
Karlsson J, Persson LO, Sjöström L, et al. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int J Obes Relat Metab Disord. 2000;24(12):1715–25. https://doi.org/10.1038/sj.ijo.0801442.
Swierz MJ, Storman D, Jasinska KW, et al. Systematic review and meta-analysis of perioperative behavioral lifestyle and nutritional interventions in bariatric surgery: a call for better research and reporting. Surg Obes Relat Dis. 2020;16(12):2088–104. https://doi.org/10.1016/j.soard.2020.08.008.
Kaiser KA, Franks S, Smith A. BH-107: Support group attendance improves post-operative weight loss. Surg Obes Relat Dis. 2009;5(3):S73.
Orth WS, Madan AK, Taddeucci RJ, et al. Support group meeting attendance is associated with better weight loss. Obes Surg. 2008;18(4):391–4. https://doi.org/10.1007/s11695-008-9444-8.
Velapati SR, Shah M, Kuchkuntla AR, et al. Weight regain after bariatric surgery: prevalence, etiology, and treatment. Curr Nutr Rep. 2018;7(4):329–34. https://doi.org/10.1007/s13668-018-0243-0.
Acknowledgements
The authors thank Roni Atzava for her collaboration in the first stages of the study design and in data collection; Orly Visid-Mizrahi and Yulia Avidor, the project coordinators; Inbal Globus, Ofri Bendrihem, Ronit Karni, Tal Cotler, Merav Dekel Dahari, Amira Dany Ben Shushan, and Sharon Malol — the supervisors of the participating support group for their assistance in data collection; Dr. Gabriel Liberman for statistical consultation; and all the participants for their cooperation. We also thank Tali Cinamon, Dr. Lisa Abarbanel Cnaani, and Billy Cohen for the support in initiating the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The study was funded by KSM (Kahn-Sagol-Maccabi), the research and innovation center of Maccabi Healthcare Services, Grant No.: 11–2017. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Participants in bariatric support groups show a significantly better self-management.
• Differences in cognitive and emotional variables between the two groups.
• These variables contribute to self-management only among support group participants.
• When possible, encourage patients to join support groups after bariatric surgery.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shinan-Altman, S., Sandbank, G.K., Natarevich–Katzav, H. et al. Self-management After Bariatric Surgery: a Comparison Between Support Group Participants and Patients Receiving Individual Dietary Follow-Up. OBES SURG 33, 826–835 (2023). https://doi.org/10.1007/s11695-022-06302-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06302-7