Abstract
Background
Health-Related Quality of Life (HRQL) is a key outcome of success after bariatric surgery. Not all patients report improved HRQL scores postoperatively, which may be due to patient-level factors. It is unknown which factors influence HRQL after surgery. Our objective was to assess patient-level factors associated with HRQL after surgery.
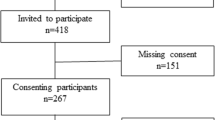
Methods
This international cross-sectional study included 730 patients who had bariatric surgery. Participants completed BODY-Q scales pertaining to HRQL and satisfaction with body, and demographic characteristics were obtained. The sample was divided into three groups based on time since surgery: 0 – 1 year, 1 – 3 years and more than 3 years. Uni- and multivariable linear regression analyses were conducted to identify variables associated with the BODY-Q scales per group.
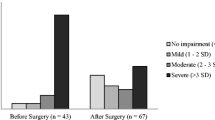
Results
The 0 – 1 year postoperative group included 377 patients (50.9%), the 1 – 3 years postoperative group 218 (29.4%) and the more than 3 years postoperative group 135 patients (18.2%). Lower current body-mass index (BMI), more weight loss (%TWL), being employed, having no comorbidities, higher age and shorter time since surgery were significantly associated with improved HRQL outcomes postoperatively. None of these factors influenced all BODY-Q scales. The effect of current BMI increased with longer time since surgery.
Conclusion
Factors including current BMI, %TWL, employment status, presence of comorbidities, age and time since surgery were associated with HRQL postoperatively. This information may be used to optimize patient-tailored care, improve patient education and underline the importance of long-term follow-up with special attention to weight regain to ensure lasting improvement in HRQL.
Graphical abstract

Similar content being viewed by others
References
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev 2014;CD003641.
Neylan CJ, Kannan U, Dempsey DT, Williams NN, Dumon KR. The surgical management of obesity. Gastroenterol Clin North Am. 2016;45(4):689–703.
Panagiotou OA, Markozannes G, Adam GP, Kowalski R, Gazula A, Di M, et al. Comparative effectiveness and safety of bariatric procedures in Medicare-eligible patients: a systematic review. JAMA Surg. 2018;153:e183326.
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11:489–506.
Coulman KD, Hopkins J, Brookes ST, Chalmers K, Main B, Owen-Smith A, et al. A core outcome set for the benefits and adverse events of bariatric and metabolic surgery: the BARIACT Project. PLOS Med. 2016;13:e1002187.
Centers for Disease Control and Prevention. Measuring healthy days: population assessment of health-related quality of life. Centers for Disease Control and Prevention; 2000. https://www.cdc.gov/hrqol/pdfs/mhd.pdf.
Weldring T, Smith SMS. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights. 2013;6:61–8.
Coulman KD, Abdelrahman T, Owen-Smith A, Andrews RC, Welbourn R, Blazeby JM. Patient-reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev. 2013;14:707–20.
Coulman KD, Blazeby JM. Health-related quality of life in bariatric and metabolic surgery. Curr Obes Rep. 2020;9:307–14.
Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017;7:273–89.
Jumbe S, Bartlett C, Jumbe SL, Meyrick J. The effectiveness of bariatric surgery on long term psychosocial quality of life—a systematic review. Obes Res Clin Pract. 2016;10:225–42.
Szmulewicz A, Wanis KN, Gripper A, Angriman F, Hawel J, Elnahas A, et al. Mental health quality of life after bariatric surgery: a systematic review and meta-analysis of randomized clinical trials. Clin Obes. 2019;9:e12290.
Rausa E, Kelly ME, Galfrascoli E, Aiolfi A, Cavalcoli F, Turati L, et al. Quality of life and gastrointestinal symptoms following laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a systematic review. Obes Surg. 2019;29:1397–402.
Flølo TN, Tell GS, Kolotkin RL, Aasprang A, Norekvål TM, Våge V, et al. Changes in quality of life 5 years after sleeve gastrectomy: a prospective cohort study. BMJ Open. 2019;9:e031170.
deMeireles AJ, Carlin AM, Bonham AJ, Cassidy R, Ross R, Stricklen A, et al. A longitudinal analysis of variation in psychological well-being and body image in patients before and after bariatric surgery. Ann Surg. 2020;271:885–90.
Dagsland V, Andenæs R, Karlsen T-I. Generic health-related quality of life may not be associated with weight loss 4 years after bariatric surgery: a cross-sectional study. Obes Surg. 2018;28:3142–50.
Monpellier VM, Antoniou EE, Aarts EO, Janssen IMC, Jansen ATM. Improvement of health-related quality of life after Roux-en-Y gastric bypass related to weight loss. Obes Surg. 2017;27:1168–73.
Sockalingam S, Hawa R, Wnuk S, Santiago V, Kowgier M, Jackson T, et al. Psychosocial predictors of quality of life and weight loss two years after bariatric surgery: results from the Toronto Bari-PSYCH study. Gen Hosp Psychiatry. 2017;47:7–13.
Khandalavala BN, Geske J, Nirmalraj M, Koran-Scholl JB, Neumann-Potash L, McBride CL. Predictors of health-related quality of life after bariatric surgery. Obes Surg. 2015;25:2302–5.
Antonsson T, Wennersten A, Sörensen K, Regnér S, Ekelund M. Differences in health-related quality of life after gastric bypass surgery: a cross-sectional study. Obes Surg. 2021;31:3194–202.
Gryth K, Persson C, Näslund I, Sundbom M, Näslund E, Stenberg E. The influence of socioeconomic factors on quality-of-life after laparoscopic gastric bypass surgery. Obes Surg. 2019;29:3569–76.
Raoof M, Szabo E, Karlsson J, Näslund E, Cao Y, Näslund I. Improvements of health-related quality of life 5 years after gastric bypass. What is important besides weight loss? A study from Scandinavian Obesity Surgery Register. Surg Obes Relat Dis. 2020;16:1249–57.
Charalampakis V, Bertsias G, Lamprou V, de Bree E, Romanos J, Melissas J. Quality of life before and after laparoscopic sleeve gastrectomy. A prospective cohort study. Surg Obes Relat Dis. 2015;11:70–6.
de Vries CEE, Kalff MC, Prinsen CAC, Coulman KD, den Haan C, Welbourn R, et al. Recommendations on the most suitable quality-of-life measurement instruments for bariatric and body contouring surgery: a systematic review. Obes Rev. 2018;19:1395–411.
de Vries CEE, Makarawung DJS, Monpellier VM, Janssen IMC, de Castro SMM, van Veen RN. Is the RAND-36 an adequate patient-reported outcome measure to assess health-related quality of life in patients undergoing bariatric surgery? Obes Surg. 2022;32(1):48–54.
Klassen AF, Cano SJ, Alderman A, Soldin M, Thoma A, Robson S, et al. The BODY-Q: a patient-reported outcome instrument for weight loss and body contouring treatments. Plast Reconstr Surg Glob Open. 2016;4:e679.
Poulsen L, Klassen A, Rose M, Roessler KK, Juhl CB, Støving RK, et al. Patient-reported outcomes in weight loss and body contouring surgery: a cross-sectional analysis using the BODY-Q. Plast Reconstr Surg. 2017;140:491–500.
Kuipers SJ, Cramm JM, Nieboer AP. The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Serv Res. 2019;19:13.
Dalaei F, Vries CEE, Poulsen L, Kaur MN, Pfob A, Mou D, et al. General population normative scores for interpreting the BODY‐Q. Clin Obes [Internet]. 2022 [cited 2022 Jun 26]; Available from: https://onlinelibrary.wiley.com/doi/10.1111/cob.12528
Klassen AF, Cano SJ, Kaur M, Breitkopf T, Pusic AL. Further psychometric validation of the BODY-Q: ability to detect change following bariatric surgery weight gain and loss. Health Qual Life Outcomes. 2017;15:227.
Poulsen L, McEvenue G, Klassen A, Hoogbergen M, Sorensen JA, Pusic A. Patient-reported outcome measures: BODY-Q. Clin Plast Surg. 2019;46:15–24.
Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg. 2016;26:395–409.
Andersen JR, Aasprang A, Karlsen T-I, Natvig GK, Våge V, Kolotkin RL. Health-related quality of life after bariatric surgery: a systematic review of prospective long-term studies. Surg Obes Relat Dis. 2015;11:466–73.
Weinberger N-A, Kersting A, Riedel-Heller SG, Luck-Sikorski C. Body dissatisfaction in individuals with obesity compared to normal-weight individuals: a systematic review and meta-analysis. Obes Facts. 2016;9:424–41.
Sarwer DB, Thompson JK, Cash TF. Body image and obesity in adulthood. Psychiatr Clin North Am. 2005;28:69–87, viii.
Tiggemann M, McCourt A. Body appreciation in adult women: relationships with age and body satisfaction. Body Image. 2013;10:624–7.
Voorwinde V, Steenhuis IHM, Janssen IMC, Monpellier VM, van Stralen MM. Definitions of long-term weight regain and their associations with clinical outcomes. Obes Surg. 2020;30:527–36.
Diener E, Lucas RE, Scollon CN. Beyond the hedonic treadmill: revising the adaptation theory of well-being. Am Psychol. 2006;61:305–14.
Hergenroeder AL, Brach JS, Otto AD, Sparto PJ, Jakicic JM. The influence of body mass index on self-report and performance-based measures of physical function in adult women. Cardiopulm Phys Ther J. 2011;22:11–20.
Rogers NT, Power C, Pinto Pereira SM. Birthweight, lifetime obesity and physical functioning in mid-adulthood: a nationwide birth cohort study. Int J Epidemiol. 2020;49:657–65.
Backholer K, Wong E, Freak-Poli R, Walls HL, Peeters A. Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta-analysis. Obes Rev. 2012;13:456–68.
McDonough CM, Jette AM. The contribution of osteoarthritis to functional limitations and disability. Clin Geriatr Med. 2010;26:387–99.
Trevisol DJ, Moreira LB, Kerkhoff A, Fuchs SC, Fuchs FD. Health-related quality of life and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens. 2011;29:179–88.
Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, Stevenson C, et al. Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1:106–14.
Peterhänsel C, Nagl M, Wagner B, Dietrich A, Kersting A. Predictors of changes in health-related quality of life 6 and 12 months after a bariatric procedure. Obes Surg. 2017;27:2120–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
‘All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards’.
Consent to Participate
‘Informed consent was obtained from all individual participants included in the study’.
Conflict of Interest
A.F. Klassen and A.L. Pusic are co-developers of the BODY-Q and, as such, obtain a share of any license revenues as royalties based on their institutions inventor sharing policy. All other authors report no relevant conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Patient-level factors such as current BMI and weight loss are associated with HRQL.
• HRQL scores are highest in the first 3 years after bariatric surgery.
• This study highlights the importance of long-term follow-up regarding weight regain.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Makarawung, D.J.S., de Vries, C.E.E., List, E.B. et al. Patient-Level Factors Associated with Health-Related Quality of Life and Satisfaction with Body After Bariatric Surgery: a Multicenter, Cross-Sectional Study. OBES SURG 32, 3079–3087 (2022). https://doi.org/10.1007/s11695-022-06214-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06214-6